Related Research Articles

Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.

Cardiac muscle is one of three types of vertebrate muscle tissues, with the other two being skeletal muscle and smooth muscle. It is an involuntary, striated muscle that constitutes the main tissue of the wall of the heart. The cardiac muscle (myocardium) forms a thick middle layer between the outer layer of the heart wall and the inner layer, with blood supplied via the coronary circulation. It is composed of individual cardiac muscle cells joined by intercalated discs, and encased by collagen fibers and other substances that form the extracellulaEditr matrix.
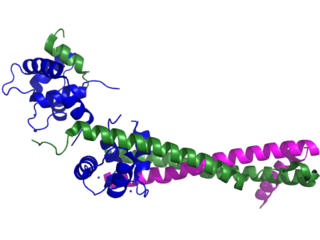
Troponin, or the troponin complex, is a complex of three regulatory proteins that are integral to muscle contraction in skeletal muscle and cardiac muscle, but not smooth muscle. Measurements of cardiac-specific troponins I and T are extensively used as diagnostic and prognostic indicators in the management of myocardial infarction and acute coronary syndrome. Blood troponin levels may be used as a diagnostic marker for stroke or other myocardial injury that is ongoing, although the sensitivity of this measurement is low.

The endocardium is the innermost layer of tissue that lines the chambers of the heart. Its cells are embryologically and biologically similar to the endothelial cells that line blood vessels. The endocardium also provides protection to the valves and heart chambers.

Intercalated discs or lines of Eberth are microscopic identifying features of cardiac muscle. Cardiac muscle consists of individual heart muscle cells (cardiomyocytes) connected by intercalated discs to work as a single functional syncytium. By contrast, skeletal muscle consists of multinucleated muscle fibers and exhibits no intercalated discs. Intercalated discs support synchronized contraction of cardiac tissue. They occur at the Z line of the sarcomere and can be visualized easily when observing a longitudinal section of the tissue.
Vasospasm refers to a condition in which an arterial spasm leads to vasoconstriction. This can lead to tissue ischemia and tissue death (necrosis). Cerebral vasospasm may arise in the context of subarachnoid hemorrhage. Symptomatic vasospasm or delayed cerebral ischemia is a major contributor to post-operative stroke and death especially after aneurysmal subarachnoid hemorrhage. Vasospasm typically appears 4 to 10 days after subarachnoid hemorrhage.
In cardiology, ventricular remodeling refers to changes in the size, shape, structure, and function of the heart. This can happen as a result of exercise or after injury to the heart muscle. The injury is typically due to acute myocardial infarction, but may be from a number of causes that result in increased pressure or volume, causing pressure overload or volume overload on the heart. Chronic hypertension, congenital heart disease with intracardiac shunting, and valvular heart disease may also lead to remodeling. After the insult occurs, a series of histopathological and structural changes occur in the left ventricular myocardium that lead to progressive decline in left ventricular performance. Ultimately, ventricular remodeling may result in diminished contractile (systolic) function and reduced stroke volume.

Unstable angina (UA), also called crescendo angina, is a type of angina pectoris that is irregular. It is also classified as a type of acute coronary syndrome (ACS).
Cardioplegia is intentional and temporary cessation of cardiac activity, primarily for cardiac surgery.
Myocardial stunning or transient post-ischemic myocardial dysfunction is a state of mechanical cardiac dysfunction that can occur in a portion of myocardium without necrosis after a brief interruption in perfusion, despite the timely restoration of normal coronary blood flow. In this situation, even after ischemia has been relieved and myocardial blood flow (MBF) returns to normal, myocardial function is still depressed for a variable period of time, usually days to weeks. This reversible reduction of function of heart contraction after reperfusion is not accounted for by tissue damage or reduced blood flow, but rather, its thought to represent a perfusion-contraction "mismatch". Myocardial stunning was first described in laboratory canine experiments in the 1970s where LV wall abnormalities were observed following coronary artery occlusion and subsequent reperfusion.

Takotsubo cardiomyopathy or Takotsubo syndrome (TTS), also known as stress cardiomyopathy, is a type of non-ischemic cardiomyopathy in which there is a sudden temporary weakening of the muscular portion of the heart. It usually appears after a significant stressor, either physical or emotional; when caused by the latter, the condition is sometimes called broken heart syndrome. Examples of physical stressors that can cause TTS are sepsis, shock, and pheochromocytoma, and emotional stressors include bereavement, divorce, or the loss of a job. Reviews suggest that of patients diagnosed with the condition, about 70–80% recently experienced a major stressor, including 41–50% with a physical stressor and 26–30% with an emotional stressor. TTS can also appear in patients who have not experienced major stressors.

Coronary ischemia, myocardial ischemia, or cardiac ischemia, is a medical term for a reduced blood flow in the coronary circulation through the coronary arteries. Coronary ischemia is linked to heart disease, and heart attacks. Coronary arteries deliver oxygen-rich blood to the heart muscle. Reduced blood flow to the heart associated with coronary ischemia can result in inadequate oxygen supply to the heart muscle. When oxygen supply to the heart is unable to keep up with oxygen demand from the muscle, the result is the characteristic symptoms of coronary ischemia, the most common of which is chest pain. Chest pain due to coronary ischemia commonly radiates to the arm or neck. Certain individuals such as women, diabetics, and the elderly may present with more varied symptoms. If blood flow through the coronary arteries is stopped completely, cardiac muscle cells may die, known as a myocardial infarction, or heart attack.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.

Contraction band necrosis is a type of uncontrolled cell death (necrosis) unique to cardiac myocytes and thought to arise in reperfusion from hypercontraction, which results in sarcolemmal rupture.
Myocardial infarction complications may occur immediately following a heart attack, or may need time to develop. After an infarction, an obvious complication is a second infarction, which may occur in the domain of another atherosclerotic coronary artery, or in the same zone if there are any live cells left in the infarct.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Management of acute coronary syndrome is targeted against the effects of reduced blood flow to the affected area of the heart muscle, usually because of a blood clot in one of the coronary arteries, the vessels that supply oxygenated blood to the myocardium. This is achieved with urgent hospitalization and medical therapy, including drugs that relieve chest pain and reduce the size of the infarct, and drugs that inhibit clot formation; for a subset of patients invasive measures are also employed. Basic principles of management are the same for all types of acute coronary syndrome. However, some important aspects of treatment depend on the presence or absence of elevation of the ST segment on the electrocardiogram, which classifies cases upon presentation to either ST segment elevation myocardial infarction (STEMI) or non-ST elevation acute coronary syndrome (NST-ACS); the latter includes unstable angina and non-ST elevation myocardial infarction (NSTEMI). Treatment is generally more aggressive for STEMI patients, and reperfusion therapy is more often reserved for them. Long-term therapy is necessary for prevention of recurrent events and complications.

Rottlerin (mallotoxin) is a polyphenol natural product isolated from the Asian tree Mallotus philippensis. Rottlerin displays a complex spectrum of pharmacology.

Ischemic cardiomyopathy is a type of cardiomyopathy caused by a narrowing of the coronary arteries which supply blood to the heart. Typically, patients with ischemic cardiomyopathy have a history of acute myocardial infarction, however, it may occur in patients with coronary artery disease, but without a past history of acute myocardial infarction. This cardiomyopathy is one of the leading causes of sudden cardiac death. The adjective ischemic means characteristic of, or accompanied by, ischemia — local anemia due to mechanical obstruction of the blood supply.

Arterial occlusion is a condition involving partial or complete blockage of blood flow through an artery. Arteries are blood vessels that carry oxygenated blood to body tissues. An occlusion of arteries disrupts oxygen and blood supply to tissues, leading to ischemia. Depending on the extent of ischemia, symptoms of arterial occlusion range from simple soreness and pain that can be relieved with rest, to a lack of sensation or paralysis that could require amputation.
References
- 1 2 3 4 Baroldi, Giorgio (2004). The Etiopathogenesis of Coronary Heart Disease: A Heretical Theory Based on Morphology, Second Edition. CRC Press. p. 88. ISBN 978-1-4987-1281-1.
- 1 2 3 4 Olsen, E. G. (2012). Atlas of Cardiovascular Pathology. Springer Science & Business Media. p. 48. ISBN 978-94-009-3209-8.
- ↑ Leone, A (2017). "Myocardial Infarction. Pathological Relevance and Relationship with Coronary Risk Factors". Current Pharmaceutical Design. 23 (22): 3205–3216. doi:10.2174/1381612823666170317123426. PMID 28317476.
- ↑ Kaur, Sarbjot; Shen, Xin; Power, Amelia; Ward, Marie-Louise (14 January 2020). "Stretch modulation of cardiac contractility: importance of myocyte calcium during the slow force response". Biophysical Reviews. 12 (1): 135–142. doi:10.1007/s12551-020-00615-6. PMC 7040129 . PMID 31939110.
- 1 2 Adegboyega, Patrick A.; Haque, Abida K.; Boor, Paul J. (November 1996). "Extensive myocytolysis as a marker of sudden cardiac death". Cardiovascular Pathology. 5 (6): 315–321. doi:10.1016/s1054-8807(96)00041-5. PMID 25851788.