Specimens
There are two major types of specimens submitted for surgical pathology analysis: biopsies and surgical resections. [1]
A biopsy is a small piece of tissue removed primarily for the purposes of surgical pathology analysis, most often in order to render a definitive diagnosis. Types of biopsies include core biopsies, which are obtained through the use of large-bore needles, sometimes under the guidance of radiological techniques such as ultrasound, CT scan, or magnetic resonance imaging. Core biopsies, which preserve tissue architecture, should not be confused with fine-needle aspiration specimens, which are analyzed using cytopathology techniques. Incisional biopsies are obtained through diagnostic surgical procedures that remove part of a suspicious lesion, whereas excisional biopsies remove the entire lesion and are similar to therapeutic surgical resections. Excisional biopsies of skin lesions and gastrointestinal polyps are very common. The pathologist's interpretation of a biopsy is critical to establishing the diagnosis of a benign or malignant tumor, and can differentiate between different types and grades of cancer, as well as determining the activity of specific molecular pathways in the tumor. This information is important for estimating the patient's prognosis and for choosing the best treatment to administer. Biopsies are also used to diagnose diseases other than cancer, including inflammatory, infectious, or idiopathic diseases of the skin and gastrointestinal tract, to name only a few.
Surgical resection specimens are obtained by the therapeutic surgical removal of an entire diseased area or organ (and occasionally multiple organs). These procedures are often intended as definitive surgical treatment of a disease in which the diagnosis is already known or strongly suspected. However, pathological analysis of these specimens is critically important in confirming the previous diagnosis, staging the extent of malignant disease, establishing whether or not the entire diseased area was removed (a process called "determination of the surgical margin", often using frozen section), identifying the presence of unsuspected concurrent diseases, and providing information for postoperative treatment, such as adjuvant chemotherapy in the case of cancer.
In the determination of surgical margin of a surgical resection, one can use the bread loafing technique, or CCPDMA. A special type of CCPDMA is named after a general surgeon, or the Mohs surgery method.

Pathology is the study of disease. The word pathology also refers to the study of disease in general, incorporating a wide range of biology research fields and medical practices. However, when used in the context of modern medical treatment, the term is often used in a narrower fashion to refer to processes and tests that fall within the contemporary medical field of "general pathology", an area that includes a number of distinct but inter-related medical specialties that diagnose disease, mostly through analysis of tissue and human cell samples. Idiomatically, "a pathology" may also refer to the predicted or actual progression of particular diseases. The suffix pathy is sometimes used to indicate a state of disease in cases of both physical ailment and psychological conditions. A physician practicing pathology is called a pathologist.

Anatomical pathology (Commonwealth) or anatomic pathology (U.S.) is a medical specialty that is concerned with the diagnosis of disease based on the macroscopic, microscopic, biochemical, immunologic and molecular examination of organs and tissues. Over the 20th century, surgical pathology has evolved tremendously: from historical examination of whole bodies (autopsy) to a more modernized practice, centered on the diagnosis and prognosis of cancer to guide treatment decision-making in oncology. Its modern founder was the Italian scientist Giovanni Battista Morgagni from Forlì.

Cytopathology is a branch of pathology that studies and diagnoses diseases on the cellular level. The discipline was founded by George Nicolas Papanicolaou in 1928. Cytopathology is generally used on samples of free cells or tissue fragments, in contrast to histopathology, which studies whole tissues. Cytopathology is frequently, less precisely, called "cytology", which means "the study of cells".

A biopsy is a medical test commonly performed by a surgeon, an interventional radiologist, or an interventional cardiologist. The process involves the extraction of sample cells or tissues for examination to determine the presence or extent of a disease. The tissue is then fixed, dehydrated, embedded, sectioned, stained and mounted before it is generally examined under a microscope by a pathologist; it may also be analyzed chemically. When an entire lump or suspicious area is removed, the procedure is called an excisional biopsy. An incisional biopsy or core biopsy samples a portion of the abnormal tissue without attempting to remove the entire lesion or tumor. When a sample of tissue or fluid is removed with a needle in such a way that cells are removed without preserving the histological architecture of the tissue cells, the procedure is called a needle aspiration biopsy. Biopsies are most commonly performed for insight into possible cancerous or inflammatory conditions.

Histopathology is the microscopic examination of tissue in order to study the manifestations of disease. Specifically, in clinical medicine, histopathology refers to the examination of a biopsy or surgical specimen by a pathologist, after the specimen has been processed and histological sections have been placed onto glass slides. In contrast, cytopathology examines free cells or tissue micro-fragments.
Dermatopathology is a joint subspecialty of dermatology and pathology or surgical pathology that focuses on the study of cutaneous diseases at a microscopic and molecular level. It also encompasses analyses of the potential causes of skin diseases at a basic level. Dermatopathologists work in close association with clinical dermatologists, with many possessing further clinical training in dermatology. The field was founded by German dermatologist and physician Gustav Simon, who published the first textbook on dermatopathology, 'Skin Diseases Illustrated by Anatomical Investigations', in 1848.

Fibroadenomas are benign breast tumours characterized by an admixture of stromal and epithelial tissue. Breasts are made of lobules and ducts. These are surrounded by glandular, fibrous and fatty tissues. Fibroadenomas develop from the lobules. The glandular tissue and ducts grow over the lobule to form a solid lump.

Fine-needle aspiration (FNA) is a diagnostic procedure used to investigate lumps or masses. In this technique, a thin, hollow needle is inserted into the mass for sampling of cells that, after being stained, are examined under a microscope (biopsy). The sampling and biopsy considered together are called fine-needle aspiration biopsy (FNAB) or fine-needle aspiration cytology (FNAC). Fine-needle aspiration biopsies are very safe minor surgical procedures. Often, a major surgical biopsy can be avoided by performing a needle aspiration biopsy instead, eliminating the need for hospitalization. In 1981, the first fine-needle aspiration biopsy in the United States was done at Maimonides Medical Center. Today, this procedure is widely used in the diagnosis of cancer and inflammatory conditions. Fine needle aspiration is generally considered a safe procedure. Complications are infrequent.

Phyllodes tumors, are a rare type of biphasic fibroepithelial mass that form from the periductal stromal and epithelial cells of the breast. They account for less than 1% of all breast neoplasms. They were previously termed cystosarcoma phyllodes, coined by Johannes Müller in 1838, before being renamed to phyllodes tumor by the World Health Organization in 2003. Phullon, which means 'leaf' in Greek, describes the unique papillary projections characteristic of phyllodes tumors on histology. Diagnosis is made via a core-needle biopsy and treatment is typically surgical resection with wide margins (>1 cm), due to their propensity to recur.

Lentigo maligna is where melanocyte cells have become malignant and grow continuously along the stratum basale of the skin, but have not invaded below the epidermis. Lentigo maligna is not the same as lentigo maligna melanoma, as detailed below. It typically progresses very slowly and can remain in a non-invasive form for years.
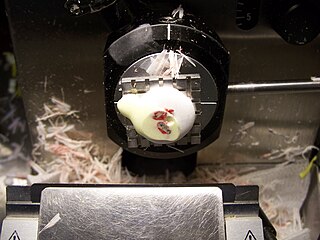
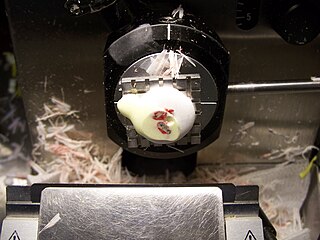
The frozen section procedure is a pathological laboratory procedure to perform rapid microscopic analysis of a specimen. It is used most often in oncological surgery. The technical name for this procedure is cryosection. The microtome device that cold cuts thin blocks of frozen tissue is called a cryotome.
An oral medicine or stomatology doctor/dentist has received additional specialized training and experience in the diagnosis and management of oral mucosal abnormalities including oral cancer, salivary gland disorders, temporomandibular disorders and facial pain, taste and smell disorders; and recognition of the oral manifestations of systemic and infectious diseases. It lies at the interface between medicine and dentistry. An oral medicine doctor is trained to diagnose and manage patients with disorders of the orofacial region.

An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life. Odontogenic keratocysts make up around 19% of jaw cysts. Despite its more common appearance in the bone region, it can affect soft tissue.
Gastrointestinal pathology is the subspecialty of surgical pathology which deals with the diagnosis and characterization of neoplastic and non-neoplastic diseases of the digestive tract and accessory organs, such as the pancreas and liver. The gastrointestinal tract is part of the digestive system or alimentary tract, and follows the passage of food and liquids as they pass through the body. The organs included in the gastrointestinal tract include the mouth, the throat (pharynx), esophagus, stomach, small intestine, large intestine, rectum and anus, in that order.

A resection margin or surgical margin is the margin of apparently non-tumorous tissue around a tumor that has been surgically removed, called "resected", in surgical oncology. The resection is an attempt to remove a cancer tumor so that no portion of the malignant growth extends past the edges or margin of the removed tumor and surrounding tissue. These are retained after the surgery and examined microscopically by a pathologist to see if the margin is indeed free from tumor cells. If cancerous cells are found at the edges the operation is much less likely to achieve the desired results.

Skin biopsy is a biopsy technique in which a skin lesion is removed to be sent to a pathologist to render a microscopic diagnosis. It is usually done under local anesthetic in a physician's office, and results are often available in 4 to 10 days. It is commonly performed by dermatologists. Skin biopsies are also done by family physicians, internists, surgeons, and other specialties. However, performed incorrectly, and without appropriate clinical information, a pathologist's interpretation of a skin biopsy can be severely limited, and therefore doctors and patients may forgo traditional biopsy techniques and instead choose Mohs surgery.

Spiradenomas (SA) are rare, benign cutaneous adnexal tumors that may progress to become their malignant counterparts, i.e. spiradenocarcinomas (SAC). Cutaneous adnexal tumors are a group of skin tumors consisting of tissues that have differentiated towards one of the four primary adnexal structures found in normal skin: hair follicles, sebaceous sweat glands, apocrine sweat glands, and eccrine sweat glands. SA and SAC tumors were regarded as eccrine gland tumors and termed eccrine spiradenomas and eccrine spiradenocarcinomas, respectively. However, more recent studies have found them to be hair follicle tumors and commonly term them spiradenomas and spiradenocarcinomas, respectively. Further confusing the situation, SA-like and SAC-like tumors are also 1) manifestations of the inherited disorder, CYLD cutaneous syndrome (CCS), and 2) have repeatedly been confused with an entirely different tumor, adenoid cystic carcinomas of the salivary gland. Here, SA and SAC are strictly defined as sporadic hair follicle tumors that do not include the hereditary CCS spiradenomas and heridtary spiradenocarcinoms of CCS or the adenoid cystic carcinomas.

Complete circumferential peripheral and deep margin assessment (CCPDMA) is the preferred method for the removal of certain cancers, especially skin cancers.

A breast biopsy is usually done after a suspicious lesion is discovered on either mammography or ultrasound to get tissue for pathological diagnosis. Several methods for a breast biopsy now exist. The most appropriate method of biopsy for a patient depends upon a variety of factors, including the size, location, appearance and characteristics of the abnormality. The different types of breast biopsies include fine-needle aspiration (FNA), vacuum-assisted biopsy, core needle biopsy, and surgical excision biopsy. Breast biopsies can be done utilizing ultrasound, MRI or a stereotactic biopsy imaging guidance. Vacuum assisted biopsies are typically done using stereotactic techniques when the suspicious lesion can only be seen on mammography. On average, 5–10 biopsies of a suspicious breast lesion will lead to the diagnosis of one case of breast cancer. Needle biopsies have largely replaced open surgical biopsies in the initial assessment of imaging as well as palpable abnormalities in the breast.

Joseph Colt Bloodgood was a prominent surgeon in the United States based in Johns Hopkins Hospital in Baltimore, Maryland. He was known for insisting on the use of rubber gloves by the entire surgical team, for advances in methods of identifying and treating benign and malignant cancers, particularly breast and bone cancers, and for advocating education of the public so they would seek routine medical examinations, even before any signs of cancer appeared.