Related Research Articles
Vascular dementia is dementia caused by a series of strokes. Restricted blood flow due to strokes reduces oxygen and glucose delivery to the brain, causing cell injury and neurological deficits in the affected region. Subtypes of vascular dementia include subcortical vascular dementia, multi-infarct dementia, stroke-related dementia, and mixed dementia.
Porencephaly is an extremely rare cephalic disorder involving encephalomalacia. It is a neurological disorder of the central nervous system characterized by cysts or cavities within the cerebral hemisphere. Porencephaly was termed by Heschl in 1859 to describe a cavity in the human brain. Derived from Greek roots, the word porencephaly means 'holes in the brain'. The cysts and cavities are more likely to be the result of destructive (encephaloclastic) cause, but can also be from abnormal development (malformative), direct damage, inflammation, or hemorrhage. The cysts and cavities cause a wide range of physiological, physical, and neurological symptoms. Depending on the patient, this disorder may cause only minor neurological problems, without any disruption of intelligence, while others may be severely disabled or die before the second decade of their lives. However, this disorder is far more common within infants, and porencephaly can occur both before or after birth.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.

Stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functioning properly.
Perinatal asphyxia is the medical condition resulting from deprivation of oxygen to a newborn infant that lasts long enough during the birth process to cause physical harm, usually to the brain. It remains a serious condition which causes significant mortality and morbidity. It is also the inability to establish and sustain adequate or spontaneous respiration upon delivery of the newborn, an emergency condition that requires adequate and quick resuscitation measures. Perinatal asphyxia is also an oxygen deficit from the 28th week of gestation to the first seven days following delivery. It is also an insult to the fetus or newborn due to lack of oxygen or lack of perfusion to various organs and may be associated with a lack of ventilation. In accordance with WHO, perinatal asphyxia is characterised by: profound metabolic acidosis, with a pH less than 7.20 on umbilical cord arterial blood sample, persistence of an Apgar score of 3 at the 5th minute, clinical neurologic sequelae in the immediate neonatal period, or evidence of multiorgan system dysfunction in the immediate neonatal period. Hypoxic damage can occur to most of the infant's organs, but brain damage is of most concern and perhaps the least likely to quickly or completely heal. In more pronounced cases, an infant will survive, but with damage to the brain manifested as either mental, such as developmental delay or intellectual disability, or physical, such as spasticity.

Cerebral hypoxia is a form of hypoxia, specifically involving the brain; when the brain is completely deprived of oxygen, it is called cerebral anoxia. There are four categories of cerebral hypoxia; they are, in order of increasing severity: diffuse cerebral hypoxia (DCH), focal cerebral ischemia, cerebral infarction, and global cerebral ischemia. Prolonged hypoxia induces neuronal cell death via apoptosis, resulting in a hypoxic brain injury.

Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.

Cerebral infarction, also known as an ischemic stroke, is the pathologic process that results in an area of necrotic tissue in the brain. In mid to high income countries, a stroke is the main reason for disability among people and the 2nd cause of death. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia). This is most commonly due to a thrombotic occlusion, or an embolic occlusion of major vessels which leads to a cerebral infarct. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.

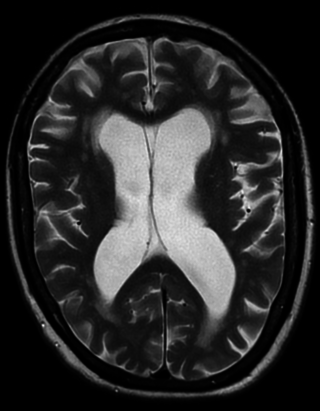
Periventricular leukomalacia (PVL) is a form of white-matter brain injury, characterized by the necrosis of white matter near the lateral ventricles. It can affect newborns and fetuses; premature infants are at the greatest risk of neonatal encephalopathy which may lead to this condition. Affected individuals generally exhibit motor control problems or other developmental delays, and they often develop cerebral palsy or epilepsy later in life. The white matter in preterm born children is particularly vulnerable during the third trimester of pregnancy when white matter developing takes place and the myelination process starts around 30 weeks of gestational age.

Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction, maternal diabetes and maternal smoking. Intrauterine growth restriction may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system. This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, attention deficit hyperactivity disorder, eating disorders and cerebral palsy.
Targeted temperature management (TTM) previously known as therapeutic hypothermia or protective hypothermia is an active treatment that tries to achieve and maintain a specific body temperature in a person for a specific duration of time in an effort to improve health outcomes during recovery after a period of stopped blood flow to the brain. This is done in an attempt to reduce the risk of tissue injury following lack of blood flow. Periods of poor blood flow may be due to cardiac arrest or the blockage of an artery by a clot as in the case of a stroke.
Neonatal encephalopathy (NE), previously known as neonatal hypoxic-ischemic encephalopathy, is defined as a encephalopathy syndrome with signs and symptoms of abnormal neurological function, in the first few days of life in an infant born after 35 weeks of gestation. In this condition there is difficulty initiating and maintaining respirations, a subnormal level of consciousness, and associated depression of tone, reflexes, and possibly seizures. Hypoxia refers to deficiency of oxygen, Ischemia refers to restriction in blood flow to the brain. The result is “encephalopathy” which refers to damaged brain cells. Encephalopathy is a nonspecific response of the brain to injury which may occur via multiple methods, but is commonly caused by birth asphyxia, leading to cerebral hypoxia.
Mild total body hypothermia, induced by cooling a baby to 33-34°C for three days after birth, is nowadays a standardized treatment after moderate to severe hypoxic ischemic encephalopathy in full-term and near to fullterm neonates. It has recently been proven to be the only medical intervention which reduces brain damage, and improves an infant's chance of survival and reduced disability.
A silent stroke is a stroke that does not have any outward symptoms associated with stroke, and the patient is typically unaware they have suffered a stroke. Despite not causing identifiable symptoms, a silent stroke still causes damage to the brain and places the patient at increased risk for both transient ischemic attack and major stroke in the future. In a broad study in 1998, more than 11 million people were estimated to have experienced a stroke in the United States. Approximately 770,000 of these strokes were symptomatic and 11 million were first-ever silent MRI infarcts or hemorrhages. Silent strokes typically cause lesions which are detected via the use of neuroimaging such as MRI. The risk of silent stroke increases with age but may also affect younger adults. Women appear to be at increased risk for silent stroke, with hypertension and current cigarette smoking being amongst the predisposing factors.
A hypothermia cap is a therapeutic device used to cool the human scalp. Its most prominent medical applications are in preventing or reducing alopecia in chemotherapy, and for preventing cerebral palsy in babies born with neonatal encephalopathy caused by hypoxic-ischemic encephalopathy (HIE). It can also be used to provide neuroprotection after cardiac arrest, to inhibit stroke paralysis, and as cryotherapy for migraine headaches.
Erythropoietin in neuroprotection is the use of the glycoprotein erythropoietin (Epo) for neuroprotection. Epo controls erythropoiesis, or red blood cell production.

Ulegyria is a diagnosis used to describe a specific type of cortical scarring in the deep regions of the sulcus that leads to distortion of the gyri. Ulegyria is identified by its characteristic "mushroom-shaped" gyri, in which scarring causes shrinkage and atrophy in the deep sulcal regions while the surface gyri are spared. This condition is most often caused by hypoxic-ischemic brain injury in the perinatal period. The effects of ulegyria can range in severity, although it is most commonly associated with cerebral palsy, mental retardation and epilepsy. N.C. Bresler was the first to view ulegyria in 1899 and described this abnormal morphology in the brain as “mushroom-gyri." Although ulegyria was first identified in 1899, there is still limited information known or reported about the condition.
A neonatal seizure is a seizure in a baby younger than age 4-weeks that is identifiable by an electrical recording of the brain. It is an occurrence of abnormal, paroxysmal, and persistent ictal rhythm with an amplitude of 2 microvolts in the electroencephalogram,. These may be manifested in form of stiffening or jerking of limbs or trunk. Sometimes random eye movements, cycling movements of legs, tonic eyeball movements, and lip-smacking movements may be observed. Alteration in heart rate, blood pressure, respiration, salivation, pupillary dilation, and other associated paroxysmal changes in the autonomic nervous system of infants may be caused due to these seizures. Often these changes are observed along with the observance of other clinical symptoms. A neonatal seizure may or may not be epileptic. Some of them may be provoked. Most neonatal seizures are due to secondary causes. With hypoxic ischemic encephalopathy being the most common cause in full term infants and intraventricular hemorrhage as the most common cause in preterm infants.
Perinatal stroke is a disease where an infant has a stroke between the 140th day of the gestation period and the 28th postpartum day, affecting up to 1 in 2300 live births. This disease is further divided into three subgroups, namely neonatal arterial ischemic stroke, neonatal cerebral sinovenous ischemic stroke, and presumed perinatal stroke. Several risk factors contribute to perinatal stroke including birth trauma, placental abruption, infections, and the mother's health.
References
- 1 2 3 4 Aden, U. (2009). Neonatal Stroke Is Not a Harmless Condition. Stroke, 40, 1948-1949. doi : 10.1161/STROKEAHA.109.550152.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Sehgal, A. (2011). Perinatal Stroke: a case-based review. European Journal of Pediatrics. doi : 10.1007/s00431-011-1509-3.
- ↑ Derugin, N., Ferriero, D. M., Vexler, Z. S. (1998) Neonatal reversible focal cerebral ischemia: a new model. Neuroscience Research 32, 349-353.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Rees, S., Harding, R., Walker, D. (2011). The biological basis of injury and neuroprotection in the fetal and neonatal brain. International Journal of Developmental Neuroscience, 29, 551-563.
- 1 2 3 4 5 6 7 8 9 10 Chauvier, D., Renolleau, S., Holifanjaniaina, S., Ankri, S., Bezault, M., Schwendimann, L., et al. (2011). Targeting neonatal ischemic brain injury with a pentapeptide-based irreversible caspase inhibitor. Cell Death & Disease, 2, 203. doi : 10.1038/cddis.2011.87.
- 1 2 3 Chabrier, S., Buchmüller, A. (2003). Editorial Comment−Specificities of the Neonatal Stroke. Stroke, 34, 2892-2893. doi : 10.1161/01.STR.0000106669.19525.0F.
- 1 2 Miller, S.P., Wu, Y.W., Lee, J., Lammer, E. J., Iovannisci, D. M., Glidden, D. V., et al.(2006). Candidate Gene Polymorphisms Do Not Differ Between Newborns With Stroke and Normal Controls. Stroke, 37, 2678-2683. doi : 10.1161/01.STR.0000244810.91105.c9.
- 1 2 Alberi, L., Chi, Z., Kadam, S. D, Mulholland, J. D., Dawson, V. L., Gaiano, N., et al. (2010). Neonatal Stroke in Mice Causes Long-Term Changes in Neuronal Notch-2 Expression That May Contribute to Prolonged Injury. Stroke, 41, 564-571. doi : 10.1161/STROKEAHA.110.595298.
- 1 2 Faustino, J. V., Wang, X., Johnson, C. E., Klibanov, A., Derugin, N., Wendland, M. F., Vexler, Z. S. (2011) Microglial cells contribute to endogenous brain defenses after acute neonatal focal stroke. The Journal of Neuroscience, 31(36), 12992-13001
- ↑ Govaert, P., Smith, L., Dudink, J. (2009) Diagnostic management of neonatal stroke. Seminars in Fetal and Neonatal Medicine, 14(5), 323-328
- ↑ Reeves, S., A., Gibbs, R., S., Clark, S., L. (2011). Magnesium for fetal neuroprotection. American Journal of Obstetrics and gynecology, 204, (3), 202.e1-202.e4
- ↑ Zeevi, B., Berant, M. (1999) Spontaneous aortic arch thrombosis in a neonate. Heart, 81, 560
- ↑ Sandberg, D. I., Lamberti-Pasculli, M., Drake, J.M., Humphreys, R. P., Rutka, J. T. (2001) Spontaneous intraparenchymal haemorrhage in full-term neonates. Neurosurgery, 48, 1042–1049.
- ↑ Himmelmann, K., Ahlin, K., Jocobsson, B., Cans, C., Thorsen, P. (2011) Risk factors for cerebral palsy in children born at term. Acta Obstetrics et Gynecologica Scandinavica,90, 1070-1081.
- 1 2 3 Westmacott, R., MacGregor, D., Askalan, R., and deVeber, G. (2009). Late Emergence of Cognitive Deficits After Unilateral Neonatal Stroke. Stroke, 40, 2012-2019. doi : 10.1161/STROKEAHA.108.533976.