Related Research Articles

Anesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. A person under the effects of anesthetic drugs is referred to as being anesthetized.

A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general anesthetic. When it is used on specific nerve pathways, paralysis also can be achieved.

General anaesthesia or general anesthesia is a medically induced coma with loss of protective reflexes, resulting from the administration of either intravenous or inhalational general anaesthetic medications, often in combination with an analgesic and neuromuscular blocking agent. It is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Combined spinal and epidural anaesthesia (CSE) is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block. The indwelling epidural catheter gives the ability to provide long lasting analgesia and to titrate the dose given to the desired effect.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés. In the United States, over 50% of childbirths involve the use of epidural anesthesia.

A thoracotomy is a surgical procedure to gain access into the pleural space of the chest. It is performed by surgeons to gain access to the thoracic organs, most commonly the heart, the lungs, or the esophagus, or for access to the thoracic aorta or the anterior spine. The purpose of a thoracotomy is the first step used to facilitate thoracic surgeries including lobectomy or pneumonectomy for lung cancer or to gain thoracic access in major trauma.

Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease feeling in a specific area. In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal's epidural space. It is available mixed with a small amount of epinephrine to increase the duration of its action. It typically begins working within 15 minutes and lasts for 2 to 8 hours.
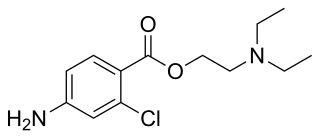
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.

Levobupivacaine (rINN) is a local anaesthetic drug belonging to the amino amide group. It is the S-enantiomer of bupivacaine.

A spinal cord stimulator (SCS) or dorsal column stimulator (DCS) is a type of implantable neuromodulation device that is used to send electrical signals to select areas of the spinal cord for the treatment of certain pain conditions. SCS is a consideration for people who have a pain condition that has not responded to more conservative therapy.
The term childbirth positions refers to the physical postures the pregnant person may assume during the process of childbirth. They may also be referred to as delivery positions or labor positions.
Andrew Gerald Doughty MRCS LRCP FRCA FRCOG was an English anaesthetist.
Dogliotti's principle is a principle in epidural anaesthesia first described by Professor Achille Mario Dogliotti in 1933. It is a method for the identification of the epidural space, a potential space. As a needle is advanced through the ligamentum flavum, to the epidural space, with constant pressure applied to the piston of a syringe, loss of resistance occurs once the needle enters the epidural space due to the change in pressure. The identification of this space, allows subsequent administration of epidural anaesthesia, a technique used primarily for analgesia during childbirth.
Post-dural-puncture headache (PDPH) is a complication of puncture of the dura mater. The headache is severe and described as "searing and spreading like hot metal", involving the back and front of the head and spreading to the neck and shoulders, sometimes involving neck stiffness. It is exacerbated by movement and sitting or standing and is relieved to some degree by lying down. Nausea, vomiting, pain in arms and legs, hearing loss, tinnitus, vertigo, dizziness and paraesthesia of the scalp are also common.

An epidural blood patch (EBP) is a surgical procedure that uses autologous blood in order to close one or many holes in the dura mater of the spinal cord, usually as a result of a previous lumbar puncture or epidural. The procedure can be used to relieve orthostatic headaches, most commonly post dural puncture headache (PDPH). The procedure carries the typical risks of any epidural procedure. They are usually administered near the site of the cerebrospinal fluid leak, but in some cases the upper part of the spine is targeted. An epidural needle is inserted into the epidural space like a traditional epidural procedure. The blood modulates the pressure of the CSF and forms a clot, sealing the leak. EBPs were first described by American anesthesiologist Turan Ozdil and surgeon James B Gormley around 1960.
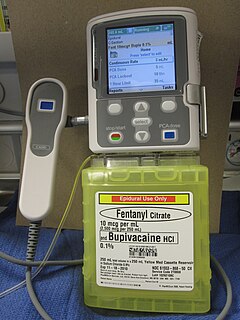
Patient-controlled analgesia (PCA) is any method of allowing a person in pain to administer their own pain relief. The infusion is programmable by the prescriber. If it is programmed and functioning as intended, the machine is unlikely to deliver an overdose of medication. Providers must always observe the first administration of any PCA medication which has not already been administered by the provider to respond to allergic reactions.

The history of neuraxial anesthesia goes back to 1885.

James Leonard Corning was an American neurologist, mainly known for his early experiments on neuraxial blockade in New York City.
Spinal extradural haematoma or spinal epidural hematoma (SEH) is bleeding into the epidural space in the spine. These may arise spontaneously, or as a rare complication of epidural anaesthesia or of surgery. Symptoms usually include back pain which radiates to the arms or the legs. They may cause pressure on the spinal cord or cauda equina, which may present as pain, muscle weakness, or dysfunction of the bladder and bowel.
References
- ↑ Brooks W (April 1957). "An epidural indicator". Anaesthesia . 12 (2): 227–228. doi: 10.1111/j.1365-2044.1957.tb03619.x . PMID 13424994.
- ↑ Iklé A (July 1950). "Preliminary report of new technique for epidural anaesthesia". British Journal of Anaesthesia . 22 (3): 150–155. doi: 10.1093/bja/22.3.150 . PMID 15426701.