Articles related to anatomy include:

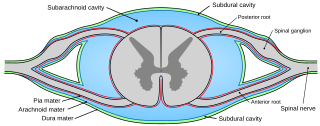
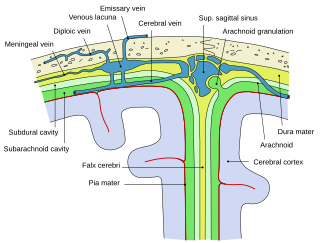
In anatomy, the meninges are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in the subarachnoid space between the arachnoid mater and the pia mater. The primary function of the meninges is to protect the central nervous system.
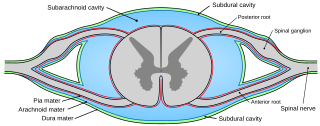
Pia mater, often referred to as simply the pia, is the delicate innermost layer of the meninges, the membranes surrounding the brain and spinal cord. Pia mater is medieval Latin meaning "tender mother". The other two meningeal membranes are the dura mater and the arachnoid mater. Both the pia and arachnoid mater are derivatives of the neural crest while the dura is derived from embryonic mesoderm. The pia mater is a thin fibrous tissue that is permeable to water and small solutes. The pia mater allows blood vessels to pass through and nourish the brain. The perivascular space between blood vessels and pia mater is proposed to be part of a pseudolymphatic system for the brain. When the pia mater becomes irritated and inflamed the result is meningitis.
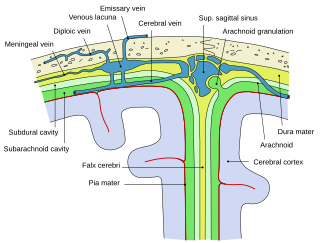
Arachnoid granulations are small outpouchings of the arachnoid mater and subarachnoid space into the dural venous sinuses of the brain. The granulations are thought to mediate the draining of cerebrospinal fluid (CSF) from the subarachnoid space into the venous system.

The dura mater, is the outermost of the three meningeal membranes. The dura mater has two layers, an outer periosteal layer closely adhered to the neurocranium, and an inner meningeal layer known as the dural border cell layer. The two dural layers are for the most part fused together forming a thick fibrous tissue membrane that covers the brain and the vertebrae of the spinal column. But the layers are separated at the dural venous sinuses to allow blood to drain from the brain. The dura covers the arachnoid mater and the pia mater the other two meninges in protecting the central nervous system.
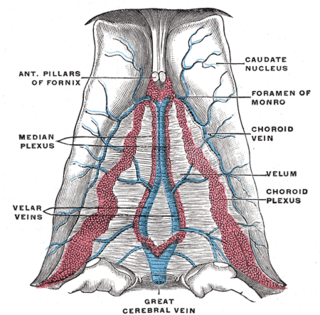
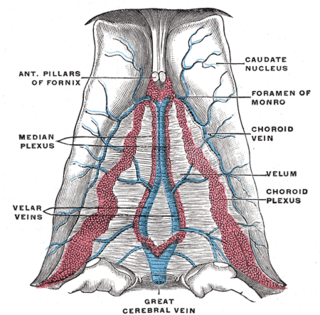
The great cerebral vein is one of the large blood vessels in the skull draining the cerebrum of the brain. It is also known as the vein of Galen, named for its discoverer, the Greek physician Galen.

A subdural hematoma (SDH) is a type of bleeding in which a collection of blood—usually but not always associated with a traumatic brain injury—gathers between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It usually results from rips in bridging veins that cross the subdural space.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

The falx cerebri is a large, crescent-shaped fold of dura mater that descends vertically into the longitudinal fissure to separate the cerebral hemispheres. It supports the dural sinuses that provide venous and CSF drainage from the brain. It is attached to the crista galli anteriorly, and blends with the tentorium cerebelli posteriorly.

The cerebellar tentorium or tentorium cerebelli is one of four dural folds that separate the cranial cavity into four (incomplete) compartments. The cerebellar tentorium separates the cerebellum from the cerebrum forming a supratentorial and an infratentorial region; the cerebrum is supratentorial and the cerebellum infratentorial.

The arachnoid mater is one of the three meninges, the protective membranes that cover the brain and spinal cord. It is so named because of its resemblance to a spider web. The arachnoid mater is a derivative of the neural crest mesoectoderm in the embryo.

The dural venous sinuses are venous sinuses (channels) found between the periosteal and meningeal layers of dura mater in the brain. They receive blood from the cerebral veins, and cerebrospinal fluid (CSF) from the subarachnoid space via arachnoid granulations. They mainly empty into the internal jugular vein. Cranial venous sinuses communicate with veins outside the skull through emissary veins. These communications help to keep the pressure of blood in the sinuses constant.
The straight sinus, also known as tentorial sinus or the sinus rectus, is an area within the skull beneath the brain. It receives blood from the inferior sagittal sinus and the great cerebral vein, and drains into the confluence of sinuses.
The superior sagittal sinus, within the human head, is an unpaired dural venous sinus lying along the attached margin of the falx cerebri. It allows blood to drain from the lateral aspects of the anterior cerebral hemispheres to the confluence of sinuses. Cerebrospinal fluid drains through arachnoid granulations into the superior sagittal sinus and is returned to the venous circulation.

The falx cerebelli is a small sickle-shaped fold of dura mater projecting forwards into the posterior cerebellar notch as well as projecting into the vallecula of the cerebellum between the two cerebellar hemispheres.
The transverse sinuses, within the human head, are two areas beneath the brain which allow blood to drain from the back of the head. They run laterally in a groove along the interior surface of the occipital bone. They drain from the confluence of sinuses to the sigmoid sinuses, which ultimately connect to the internal jugular vein. See diagram : labeled under the brain as "SIN. TRANS.".

The intervertebral foramen is an opening between two pedicles of adjacent vertebra in the articulated spine. Each intervertebral foramen gives passage to a spinal nerve and spinal blood vessels, and lodges a posterior (dorsal) root ganglion. Cervical, thoracic, and lumbar vertebrae all have intervertebral foramina.
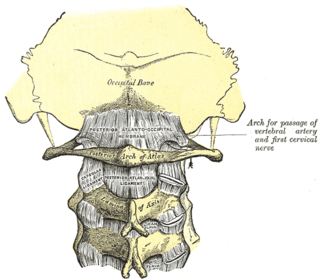
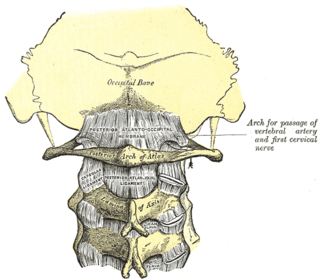
The posterior atlantooccipital membrane is a broad but thin membrane extending between the posterior margin of the foramen magnum above, and posterior arch of atlas below. It forms the floor of the suboccipital triangle.

The calvaria is the top part of the skull. It is the superior part of the neurocranium and covers the cranial cavity containing the brain. It forms the main component of the skull roof.
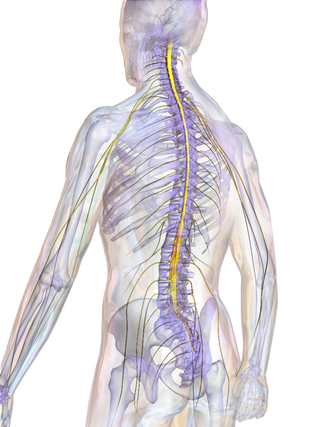
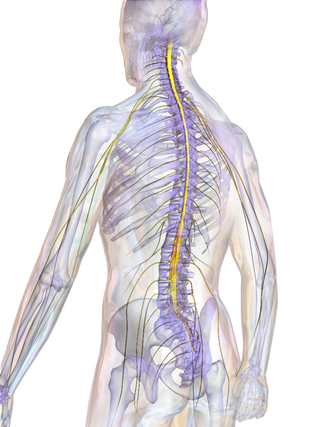
The spinal cord is a long, thin, tubular structure made up of nervous tissue that extends from the medulla oblongata in the lower brainstem to the lumbar region of the vertebral column (backbone) of vertebrate animals. The center of the spinal cord is hollow and contains a structure called the central canal, which contains cerebrospinal fluid. The spinal cord is also covered by meninges and enclosed by the neural arches. Together, the brain and spinal cord make up the central nervous system.