Related Research Articles

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.

A local anesthetic (LA) is a medication that causes absence of all sensation in a specific body part without loss of consciousness, providing local anesthesia, as opposed to a general anesthetic, which eliminates all sensation in the entire body and causes unconsciousness. Local anesthetics are most commonly used to eliminate pain during or after surgery. When it is used on specific nerve pathways, paralysis also can be induced.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true anaesthesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Combined spinal and epidural anaesthesia is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block. The indwelling epidural catheter gives the ability to provide long lasting analgesia and to titrate the dose given to the desired effect.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

Arachnoiditis is an inflammatory condition of the arachnoid mater or 'arachnoid', one of the membranes known as meninges that surround and protect the central nervous system. The outermost layer of the meninges is the dura mater and adheres to inner surface of the skull and vertebrae. The arachnoid is under or "deep" to the dura and is a thin membrane that adheres directly to the surface of the brain and spinal cord.
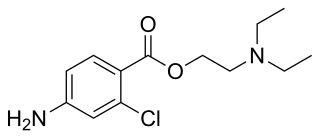
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.
Dogliotti's principle is a principle in epidural anaesthesia first described by Professor Achille Mario Dogliotti in 1933. It is a method for the identification of the epidural space, a potential space. As a needle is advanced through the ligamentum flavum, to the epidural space, with constant pressure applied to the piston of a syringe, loss of resistance occurs once the needle enters the epidural space due to the change in pressure. The identification of this space, allows subsequent administration of epidural anaesthesia, a technique used primarily for analgesia during childbirth.

Post-dural-puncture headache (PDPH) is a complication of puncture of the dura mater. The headache is severe and described as "searing and spreading like hot metal", involving the back and front of the head and spreading to the neck and shoulders, sometimes involving neck stiffness. It is exacerbated by movement and sitting or standing and is relieved to some degree by lying down. Nausea, vomiting, pain in arms and legs, hearing loss, tinnitus, vertigo, dizziness and paraesthesia of the scalp are also common.

An epidural blood patch (EBP) is a surgical procedure that uses autologous blood, meaning the patient's own blood, in order to close one or many holes in the dura mater of the spinal cord, which occurred as a complication of a lumbar puncture or epidural placement. The punctured dura causes cerebrospinal fluid leak. The procedure can be used to relieve orthostatic headaches, most commonly post dural puncture headache (PDPH).

Eugen Bogdan Aburel was a Romanian surgeon and obstetrician. He introduced innovative techniques in gynecologic surgery.
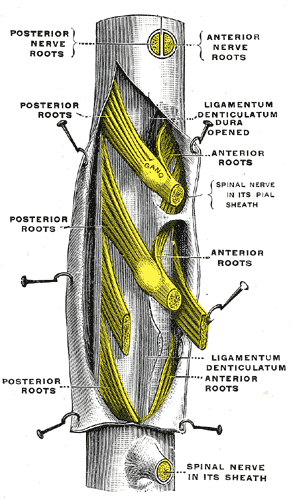
The thecal sac or dural sac is the membranous sheath (theca) or tube of dura mater that surrounds the spinal cord and the cauda equina. The thecal sac contains the cerebrospinal fluid which provides nutrients and buoyancy to the spinal cord. From the skull the tube adheres to bone at the foramen magnum and extends down to the second sacral vertebra where it tapers to cover over the filum terminale. Along most of the spinal canal it is separated from the inner surface by the epidural space. The sac has projections that follow the spinal nerves along their paths out of the vertebral canal which become the dural root sheaths.
Continuous wound infiltration (CWI) refers to the continuous infiltration of a local anesthetic into a surgical wound to aid in pain management during post-operative recovery.

Fidel Pagés Miravé was a Spanish military surgeon, known for developing the technique of epidural anesthesia.
The following outline is provided as an overview of and topical guide to anesthesia:
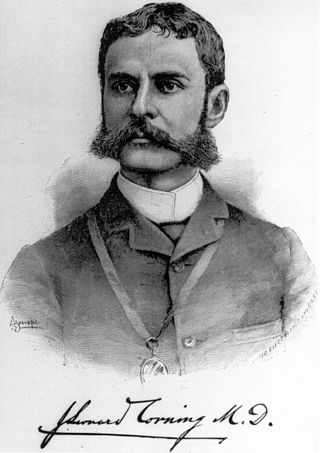
The history of neuraxial anaesthesia dates back to the late 1800s and is closely intertwined with the development of anaesthesia in general. Neuraxial anaesthesia, in particular, is a form of regional analgesia placed in or around the Central Nervous System, used for pain management and anaesthesia for certain surgeries and procedures.
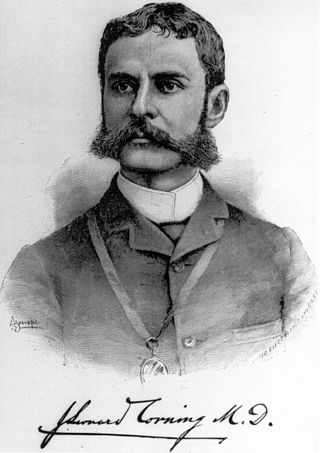
James Leonard Corning was an American neurologist, mainly known for his early experiments on neuraxial blockade in New York City.
Obstetric anesthesia or obstetric anesthesiology, also known as ob-gyn anesthesia or ob-gyn anesthesiology, is a sub-specialty of anesthesiology that provides peripartum pain relief (analgesia) for labor and anesthesia for cesarean deliveries ('C-sections').

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults, it can be used in the context of anorectal surgery or for chronic low back pain management.
References
- ↑ Miller's Anesthesia (8 ed.). Elsevier. 2015. pp. 1684–1720.
- ↑ Ituk, Unyime; Wong, Cynthia A (2022). "Overview of neuraxial anesthesia" . UpToDate . Philadelphia: Wolters Kluwer. Retrieved 18 December 2022.
- ↑ Basics of Anesthesia (7 ed.). Elsevier. 2018. pp. 272–302.