Related Research Articles

Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.

Laryngoscopy is endoscopy of the larynx, a part of the throat. It is a medical procedure that is used to obtain a view, for example, of the vocal folds and the glottis. Laryngoscopy may be performed to facilitate tracheal intubation during general anaesthesia or cardiopulmonary resuscitation or for surgical procedures on the larynx or other parts of the upper tracheobronchial tree.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory, it is also possible for the victim to have awareness with explicit recall, where victims can remember the events related to their surgery.

Ropivacaine (rINN) is a local anaesthetic drug belonging to the amino amide group. The name ropivacaine refers to both the racemate and the marketed S-enantiomer. Ropivacaine hydrochloride is commonly marketed by AstraZeneca under the brand name Naropin.

Atracurium besilate, also known as atracurium besylate, is a medication used in addition to other medications to provide skeletal muscle relaxation during surgery or mechanical ventilation. It can also be used to help with endotracheal intubation but suxamethonium (succinylcholine) is generally preferred if this needs to be done quickly. It is given by injection into a vein. Effects are greatest at about 4 minutes and last for up to an hour.
Alfaxolone/alfadolone (brand names Althesin, Saffan is a short acting intravenous anaesthetic agent. It was withdrawn from the market due to severe drug reactions. It is composed of a 3:1 mixture of alfaxalone and alfadolone, two neurosteroids.
The ASA physical status classification system is a system for assessing the fitness of patients before surgery. In 1963 the American Society of Anesthesiologists (ASA) adopted the five-category physical status classification system; a sixth category was later added. These are:
- Healthy person.
- Mild systemic disease.
- Severe systemic disease.
- Severe systemic disease that is a constant threat to life.
- A moribund person who is not expected to survive without the operation.
- A declared brain-dead person whose organs are being removed for donor purposes.
Odom's indicator is a device used for locating the epidural space in regional anaesthesia. The device works on Dogliotti's principle by finding an area of decreased resistance to injection. It was originally designed on the assumption that the pressure in the epidural space was negative. This device is no-longer popular and alternative methods are now used.
Dogliotti's principle is a principle in epidural anaesthesia first described by Professor Achille Mario Dogliotti in 1933. It is a method for the identification of the epidural space, a potential space. As a needle is advanced through the ligamentum flavum, to the epidural space, with constant pressure applied to the piston of a syringe, loss of resistance occurs once the needle enters the epidural space due to the change in pressure. The identification of this space, allows subsequent administration of epidural anaesthesia, a technique used primarily for analgesia during childbirth.
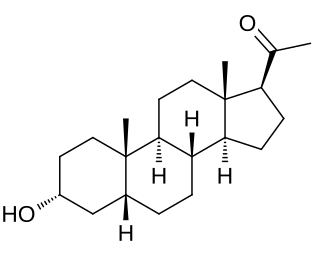
Pregnanolone, also known as eltanolone, is an endogenous inhibitory neurosteroid which is produced in the body from progesterone. It is closely related to allopregnanolone, which has similar properties.

Propofol infusion syndrome (PRIS) is a rare syndrome which affects patients undergoing long-term treatment with high doses of the anaesthetic and sedative drug propofol. It can lead to cardiac failure, rhabdomyolysis, metabolic acidosis, and kidney failure, and is often fatal. High blood potassium, high blood triglycerides, and liver enlargement, proposed to be caused by either "a direct mitochondrial respiratory chain inhibition or impaired mitochondrial fatty acid metabolism" are also key features. It is associated with high doses and long-term use of propofol. It occurs more commonly in children, and critically ill patients receiving catecholamines and glucocorticoids are at high risk. Treatment is supportive. Early recognition of the syndrome and discontinuation of the propofol infusion reduces morbidity and mortality.

In anesthesia, neuromuscular blocking agents may be required to facilitate endotracheal intubation and provide optimal surgical conditions. When neuromuscular blocking agents are administered, neuromuscular function of the patient must be monitored. Neuromuscular function monitoring is a technique that involves the electrical stimulation of a motor nerve and monitoring the response of the muscle supplied by that nerve. It may be used from the induction of to recovery from neuromuscular blockade. Importantly, it is used to confirm adequacy of recovery after the administration of neuromuscular blocking agents. The response of the muscles to electrical stimulation of the nerves can be recorded subjectively (qualitative) or objectively (quantitatively). Quantitative techniques include electromyography, acceleromyography, kinemyography, phonomygraphy and mechanomyography. Neuromuscular monitoring is recommended when neuromuscular-blocking drugs have been part of the general anesthesia and the doctor wishes to avoid postoperative residual curarization (PORC) in the patient, that is, the residual paralysis of muscles stemming from these drugs.

Postoperative residual curarization (PORC) or residual neuromuscular blockade (RNMB) is a residual paresis after emergence from general anesthesia that may occur with the use of neuromuscular-blocking drugs. Today residual neuromuscular blockade is defined as a train of four ratio of less than 0.9 when measuring the response to ulnar nerve stimulation at the adductor pollicis muscle using mechanomyography or electromyography. A meta-analysis reported that the incidence of residual neuromuscular paralysis was 41% in patients receiving intermediate neuromuscular blocking agents during anaesthesia. It is possible that > 100,000 patients annually in the USA alone, are at risk of adverse events associated with undetected residual neuromuscular blockade. Neuromuscular function monitoring and the use of the appropriate dosage of sugammadex to reverse blockade produced by rocuronium can reduce the incidence of postoperative residual curarization. In this study, with usual care group receiving reversal with neostigmine resulted in a residual blockade rate of 43%.
The Cormack-Lehane system classifies views obtained by direct laryngoscopy based on the structures seen. It was initially described by R.S. Cormack and J. Lehane in 1984 as a way of simulating potential scenarios that trainee anaesthetists might face. A modified version that subdivided Grade 2 was initially described in 1998.
Percutaneous transtracheal ventilation is the delivery of oxygen to the lungs through an over-the-needle catheter inserted through the skin into the trachea using a high pressure gas source is considered a form of conventional ventilation.

The laryngeal tube is an airway management device designed as an alternative to other airway management techniques such as mask ventilation, laryngeal mask airway, and tracheal intubation. This device can be inserted blindly through the oropharynx into the hypopharynx to create an airway during anaesthesia and cardiopulmonary resuscitation so as to enable mechanical ventilation of the lungs.

Airtraq is a fibreoptic intubation device used for indirect tracheal intubation in difficult airway situations. It is designed to enable a view of the glottic opening without aligning the oral with the pharyngeal, and laryngeal axes as an advantage over direct endotracheal intubation and allows for intubation with minimal head manipulation and positioning.
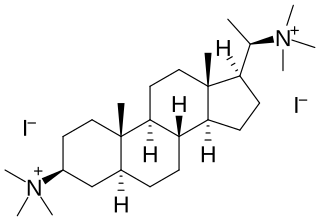
Malouetine is an aminosteroid neuromuscular blocking agent and antinicotinic alkaloid isolated from Malouetia spp.
Thyromental distance (TMD) measurement is a method commonly used to predict the difficulty of intubation and is measured from the thyroid notch to the tip of the jaw with the head extended. If it is less than 7.0 cm with hard scarred tissues, it indicates possible difficult intubation.
A transverse abdominis plane block, also called TAP block, is a regional technique to provide analgesia after lower abdominal wall operations. The techniques was first introduced by Rafi in 2001. It is performed using local anesthetic agent mostly Ropivacaine, Bupivacaine but block does not last longer compared to when given with new drug Liposomal bupivacaine. There are multiple studies confirming liposomal bupivacaine TAP block is effective for up to 72 hours after the surgery. Citation???
References
- Dravid, RM; Paul, RE (Oct 2007). "Interpleural block - part 1". Anaesthesia. 62 (10): 1039–49. doi: 10.1111/j.1365-2044.2007.05183.x . PMID 17845657.
- Dravid, RM; Paul, RE (Nov 2007). "Interpleural block - part 2". Anaesthesia. 62 (11): 1143–53. doi:10.1111/j.1365-2044.2007.05181.x. PMID 17924896. S2CID 13577711.