Related Research Articles

Anesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.
Chloroform, or trichloromethane (often abbreviated as TCM), is an organic compound with the formula CHCl3 and a common organic solvent. It is a very volatile, colorless, strong-smelling, dense liquid produced on a large scale as a precursor to PTFE and refrigerants and is a trihalomethane that serves as a powerful anesthetic, euphoriant, anxiolytic, and sedative when inhaled or ingested. Chloroform was frequently used as an anaesthetic between 1847 and the first half of the 20th century. It is also part of a wider class of substances known as volatile organic compounds. Chloroform is miscible with many solvents but it is only very slightly soluble in water (only 8 g/L at 20 °C).

Isoflurane, sold under the brand name Forane among others, is a general anesthetic. It can be used to start or maintain anesthesia; however, other medications are often used to start anesthesia, due to airway irritation with isoflurane. Isoflurane is given via inhalation.

General anaesthesia (UK) or general anesthesia (US) is a medically induced loss of consciousness that renders the patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients.

Anesthesiology, anaesthesiology, or anaesthesia is the medical specialty concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialized in anesthesiology is called an anesthesiologist, anaesthesiologist, or anaesthetist, depending on the country. In some countries, the terms are synonymous, while in other countries they refer to different positions, and anesthetist is only used for non-physicians, such as nurse anesthetists.

An inhalational anesthetic is a chemical compound possessing general anesthetic properties that can be delivered via inhalation. They are administered through a face mask, laryngeal mask airway or tracheal tube connected to an anesthetic vaporiser and an anesthetic delivery system. Agents of significant contemporary clinical interest include volatile anesthetic agents such as isoflurane, sevoflurane and desflurane, as well as certain anesthetic gases such as nitrous oxide and xenon.
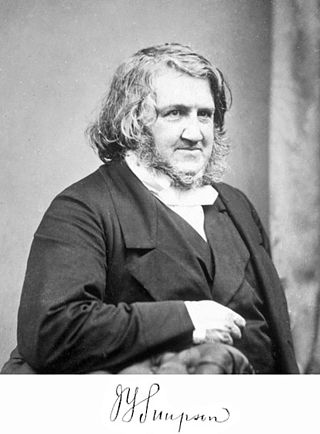
Sir James Young Simpson, 1st Baronet, was a Scottish obstetrician and a significant figure in the history of medicine. He was the first physician to demonstrate the anaesthetic properties of chloroform on humans and helped to popularise its use in medicine.
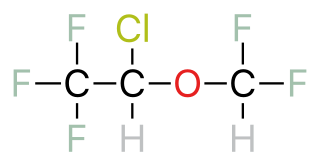
A halogenated ether is a subcategory of a larger group of chemicals known as ethers. An ether is an organic chemical that contains an ether group—an oxygen atom connected to two (substituted) alkyl groups. A good example of an ether is the solvent diethyl ether.
Minimum alveolar concentration or MAC is the concentration, often expressed as a percentage by volume, of a vapour in the alveoli of the lungs that is needed to prevent movement in 50% of subjects in response to surgical (pain) stimulus. MAC is used to compare the strengths, or potency, of anaesthetic vapours. The concept of MAC was first introduced in 1965.

Methoxyflurane, sold under the brand name Penthrox among others, is an inhaled medication primarily used to reduce pain following trauma. It may also be used for short episodes of pain as a result of medical procedures. Onset of pain relief is rapid and of a short duration. Use is only recommended with direct medical supervision.
Curt Theodor Schimmelbusch was a German physician and pathologist who invented the Schimmelbusch mask, for the safe delivery of anaesthetics to surgical patients. He was also a key figure in the development of mechanical methods of sterilisation and disinfection for surgical procedures, on which his Anleitung zur aseptischen Wundbehandlung was considered a seminal work.

Joseph Thomas Clover was an English doctor and pioneer of anaesthesia. He invented a variety of pieces of apparatus to deliver anaesthetics including ether and chloroform safely and controllably. By 1871 he had administered anaesthetics 13,000 times without a fatality.

Throughout recorded history, attempts at producing a state of general anesthesia can be traced back to the writings of ancient Sumerians, Babylonians, Assyrians, Egyptians, Indians, and Chinese. Despite significant advances in anatomy and surgical technique during the Renaissance, surgery remained a last-resort treatment largely due to the pain associated with it. However, scientific discoveries in the late 18th and early 19th centuries paved the way for the development of modern anesthetic techniques.
The Chloroform Committee was commissioned by the Royal Medical and Chirurgical Society in 1864 to investigate the use of chloroform. The committee recommended the use of chloroform in the same year. It was the first of such committees and concluded that chloroform depresses the action of the heart and frequently kills. One of the members, Joseph Clover, during his time on the committee developed apparatus for using chloroform called the Clover bag.
The Special Chloroform Committee of the British Medical Association was established in 1901 following the annual meeting of the British Medical Association and it produced its last final report 1910.

An anesthetic vaporizer or anaesthetic vaporiser is a device generally attached to an anesthetic machine which delivers a given concentration of a volatile anesthetic agent. It works by controlling the vaporization of anesthetic agents from liquid, and then accurately controlling the concentration in which these are added to the fresh gas flow. The design of these devices takes account of varying: ambient temperature, fresh gas flow, and agent vapor pressure.
George Warwick Bampfylde Daniell (1864–1937) was medical practitioner and anaesthesiologist who practised in South Africa in the 19th and 20th centuries.
Obstetric anesthesia or obstetric anesthesiology, also known as ob-gyn anesthesia or ob-gyn anesthesiology, is a sub-specialty of anesthesiology that provides peripartum pain relief (analgesia) for labor and anesthesia for cesarean deliveries ('C-sections').

Nathaniel H. Alcock was an Irish medical doctor.

James Robinson was a British dentist and anaesthetist. On 19 December 1846, he became the first person to carry out general anaesthesia in Britain when he administered ether to a patient undergoing a tooth extraction. The next year, he published A Treatise on the Inhalation of the Vapour of Ether, perhaps the first textbook of anaesthesia. Robinson's work influenced the prominent anaesthetist John Snow. Robinson also undertook initiatives to reform the dental profession in Britain. At the age of 48, he died of blood loss following a gardening accident; his London home, as well as the site where he first administered anaesthesia, are commemorated with plaques.
References
- 1 2 3 4 5 6 Wilmot Buxton, Dudley (2009-12-09). Anaesthetics - Their Uses and Administration (Reprint of the first edition - 1888). Read Books. pp. 332–340. ISBN 978-1-4446-9013-2.
- 1 2 3 Wawersik, Juergen (1991). "History of anesthesia in Germany". Journal of Clinical Anesthesia. 3 (3): 235–244. doi:10.1016/0952-8180(91)90167-L. PMID 1878238.
- ↑ "Everybody" (pseudonym) (1935). Everybody's Family Doctor. London: Odhams Press. p. 11. OCLC 558994903.
- ↑ Mccardie, WJ (1898-12-17). "On the administration of a certain mixture of chloroform and ether in gynecological operations by means of a Clover's inhaler without the bag". The Lancet. 152 (3929): 1621–1624. doi:10.1016/S0140-6736(01)84517-7.
- 1 2 3 "Deaths under chloroform And A.C.E. mixture". The British Medical Journal. 2 (1663): 1072–1073. 1892-11-12. JSTOR 20222445.
- 1 2 "Death Under Chloroform". The British Medical Journal. 2 (1698): 143. 1893-07-15. doi:10.1136/bmj.2.1698.152. JSTOR 20225168. S2CID 1432522.
- ↑ Simpson, J. Christian (1890-08-30). "Alcohol In Anæsthetic Mixtures". The British Medical Journal. 2 (1548): 529. doi:10.1136/bmj.2.1185.529. JSTOR 20240176. S2CID 12472582.
- ↑ Walters, J (1887-11-12). "A. C. E. Mixture". The British Medical Journal. 2 (1402): 1078. doi:10.1136/bmj.2.1402.1078-a. JSTOR 20213635. S2CID 73074361.
- ↑ "Deaths Under Anæsthetics. A.C.E. Mixture". The British Medical Journal. 1 (1779): 282. 1895-02-02. doi:10.1136/bmj.1.2666.282. JSTOR 20231460. PMC 2344476 .
- ↑ Levy, AG (October 13, 1923). "Ether Versus Chloroform". The British Medical Journal. 2 (3276): 681. doi:10.1136/bmj.2.1447.681. JSTOR 20434527. S2CID 220195762.
- ↑ Stephens, William J. (1888-01-07). "A Pleasant Anæsthetic Mixture". The British Medical Journal. 1 (1410): 19. doi:10.1136/bmj.1.105.19. JSTOR 20214092. S2CID 34144846.
- ↑ British Journal of Dental Science and Prosthetics. (1883). UK: J. P. Segg & Company., p. 692
- ↑ "Royal Commission On Vivisection. Fifth Report (Continued)". The British Medical Journal. 2 (2481): 159–162. 1908-07-18. doi:10.1136/bmj.2.3577.159-a. JSTOR 25278404. S2CID 220149652.