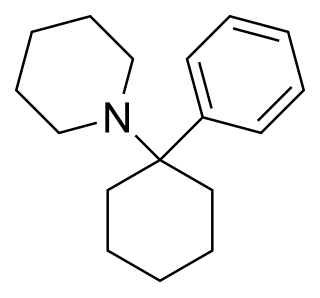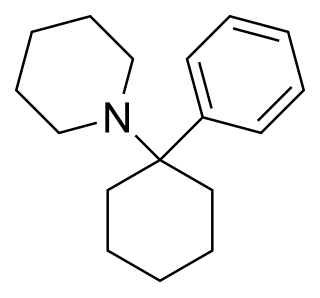
Phencyclidine or phenylcyclohexyl piperidine (PCP), also known in its use as a street drug as angel dust among other names, is a dissociative anesthetic mainly used recreationally for its significant mind-altering effects. PCP may cause hallucinations, distorted perceptions of sounds, and violent behavior. As a recreational drug, it is typically smoked, but may be taken by mouth, snorted, or injected. It may also be mixed with cannabis or tobacco.

The N-methyl-D-aspartatereceptor (also known as the NMDA receptor or NMDAR), is a glutamate receptor and ion channel found in neurons. The NMDA receptor is one of three types of ionotropic glutamate receptors, the other two being AMPA and kainate receptors. Depending on its subunit composition, its ligands are glutamate and glycine (or D-serine). However, the binding of the ligands is typically not sufficient to open the channel as it may be blocked by Mg2+ ions which are only removed when the neuron is sufficiently depolarized. Thus, the channel acts as a “coincidence detector” and only once both of these conditions are met, the channel opens and it allows positively charged ions (cations) to flow through the cell membrane. The NMDA receptor is thought to be very important for controlling synaptic plasticity and mediating learning and memory functions.

A dopamine antagonist, also known as an anti-dopaminergic and a dopamine receptor antagonist (DRA), is a type of drug which blocks dopamine receptors by receptor antagonism. Most antipsychotics are dopamine antagonists, and as such they have found use in treating schizophrenia, bipolar disorder, and stimulant psychosis. Several other dopamine antagonists are antiemetics used in the treatment of nausea and vomiting.

Glutamate receptors are synaptic and non synaptic receptors located primarily on the membranes of neuronal and glial cells. Glutamate is abundant in the human body, but particularly in the nervous system and especially prominent in the human brain where it is the body's most prominent neurotransmitter, the brain's main excitatory neurotransmitter, and also the precursor for GABA, the brain's main inhibitory neurotransmitter. Glutamate receptors are responsible for the glutamate-mediated postsynaptic excitation of neural cells, and are important for neural communication, memory formation, learning, and regulation.

NMDA receptor antagonists are a class of drugs that work to antagonize, or inhibit the action of, the N-Methyl-D-aspartate receptor (NMDAR). They are commonly used as anesthetics for animals and humans; the state of anesthesia they induce is referred to as dissociative anesthesia.
The glutamate hypothesis of schizophrenia models the subset of pathologic mechanisms of schizophrenia linked to glutamatergic signaling. The hypothesis was initially based on a set of clinical, neuropathological, and, later, genetic findings pointing at a hypofunction of glutamatergic signaling via NMDA receptors. While thought to be more proximal to the root causes of schizophrenia, it does not negate the dopamine hypothesis, and the two may be ultimately brought together by circuit-based models. The development of the hypothesis allowed for the integration of the GABAergic and oscillatory abnormalities into the converging disease model and made it possible to discover the causes of some disruptions.

Xanomeline is a small molecule muscarinic acetylcholine receptor agonist that was first synthesized in a collaboration between Eli Lilly and Novo Nordisk as an investigational therapeutic being studied for the treatment of central nervous system disorders.
NMDA receptor modulators are a new form of antipsychotic that are in Phase II FDA studies. The first compound studied was glycine which was hypothesized by Daniel Javitt after observation that people with phencyclidine(PCP)-induced psychosis were lacking in glutamate transmission. In giving glycine to people with PCP-induced psychosis a recovery rate was noted. From there, it was hypothesized that people with psychosis from schizophrenia would benefit from increased glutamate transmission and glycine was added with strong recovery rates noted especially in the area of negative and cognitive symptoms. Glycine, however, sporadic results aside remains an adjunct antipsychotic and an unworkable compound. However, the Eli Lilly and Company study drug LY-2140023 is being studied as a primary antipsychotic and is showing strong recovery rates, especially in the area of negative and cognitive symptoms of schizophrenia. Tardive dyskinesia, diabetes and other standard complications have not been noted:
Treatment with LY2140023, like treatment with olanzapine, was safe and well-tolerated; treated patients showed statistically significant improvements in both positive and negative symptoms of schizophrenia compared to placebo. Notably, patients treated with LY-2140023 did not differ from placebo-treated patients with respect to prolactin elevation, extrapyramidal symptoms or weight gain. These data suggest that mGlu2/3 receptor agonists have antipsychotic properties and may provide a new alternative for the treatment of schizophrenia.

Pomaglumetad (LY-404,039) is an amino acid analog drug that acts as a highly selective agonist for the metabotropic glutamate receptor group II subtypes mGluR2 and mGluR3. Pharmacological research has focused on its potential antipsychotic and anxiolytic effects. Pomaglumetad is intended as a treatment for schizophrenia and other psychotic and anxiety disorders by modulating glutamatergic activity and reducing presynaptic release of glutamate at synapses in limbic and forebrain areas relevant to these disorders. Human studies investigating therapeutic use of pomaglumetad have focused on the prodrug LY-2140023, a methionine amide of pomaglumetad (also called pomaglumetad methionil) since pomaglumetad exhibits low oral absorption and bioavailability in humans.

CDPPB is a drug used in scientific research which acts as a positive allosteric modulator selective for the metabotropic glutamate receptor subtype mGluR5. It has antipsychotic effects in animal models, and mGluR5 modulators are under investigation as potential drugs for the treatment of schizophrenia, as well as other applications.

Sunifiram is an experimental drug which has antiamnesic effects in animal studies and with significantly higher potency than piracetam. Sunifiram is a molecular simplification of unifiram (DM-232). Another analogue is sapunifiram (MN-19). As of 2016, sunifiram had not been subjected to toxicology testing, nor to any human clinical trials, and is not approved for use anywhere in the world.

Indantadol is a drug which was formerly being investigated as an anticonvulsant and neuroprotective and is now under development for the treatment of neuropathic pain and chronic cough in Europe by Vernalis and Chiesi. It acts as a competitive, reversible, and non-selective monoamine oxidase inhibitor, and as a low affinity, non-competitive NMDA receptor antagonist. A pilot study of indantadol for chronic cough was initiated in October 2009 and in April 2010 it failed to achieve significant efficacy in neuropathic pain in phase IIb clinical trials.

ORG-25935, also known as SCH-900435 is a synthetic drug developed by Organon International, which acts as a selective inhibitor of the glycine transporter GlyT-1. In animal tests it reduces alcohol consumption and has analgesic and anticonvulsant effects, but it has mainly been studied for its antipsychotic properties, and in human trials it was shown to effectively counteract the effects of the dissociative drug ketamine.

Rapastinel is a novel antidepressant that was under development by Allergan as an adjunctive therapy for the treatment of treatment-resistant depression. It is a centrally active, intravenously administered amidated tetrapeptide that acts as a novel and selective modulator of the NMDA receptor. The drug is a rapid-acting and long-lasting antidepressant as well as robust cognitive enhancer by virtue of its ability to enhance NMDA receptor-mediated signal transduction and synaptic plasticity.

Apimostinel is an investigational antidepressant, acting as a novel and selective modulator of the NMDA receptor. It is currently under development for the acute treatment of major depressive disorder (MDD) by Gate Neurosciences, and previously by Naurex and Allergan. As of February 2015, an intravenous formulation of apimostinel has completed a phase IIa clinical trial for MDD.

Brilaroxazine, also known as oxaripiprazole, is an investigational atypical antipsychotic which is under development by Reviva Pharmaceuticals for the treatment of neuropsychiatric and inflammatory disorders. It has currently completed the first of two phase III clinical trials for schizophrenia. Reviva Pharmaceuticals also intends to investigate brilaroxazine for the treatment of bipolar disorder, major depressive disorder, attention deficit hyperactivity disorder (ADD/ADHD), psychosis/agitation associated with Alzheimer's disease, Parkinson's disease psychosis, as well as the inflammatory disorders pulmonary arterial hypertension (PAH), idiopathic pulmonary fibrosis (IPF), and psoriasis. The FDA granted brilaroxazine orphan drug designation for the treatment of PAH and IPF.

Pesampator is a positive allosteric modulator (PAM) of the AMPA receptor (AMPAR), an ionotropic glutamate receptor, which is under development by Pfizer for the treatment of cognitive symptoms in schizophrenia. It was also under development for the treatment of age-related sensorineural hearing loss, but development for this indication was terminated due to insufficient effectiveness. As of July 2018, pesampator is in phase II clinical trials for cognitive symptoms in schizophrenia.

Iclepertin is an investigational nootropic to enhance the cognition and functional capacity in schizophrenia developed by Boehringer Ingelheim. As of May 2020, it is in phase III of clinical trial under the code name CONNEX-3. BI 425809 is an inhibitor of glycine transporter 1 (Gly-T1) that in phase II improved cognition after 12 weeks in patients with schizophrenia. Doses of 10 mg and 25 mg showed the largest separation from placebo. If these encouraging results are confirmed in phase 3 trials, BI 425809 could provide an effective treatment for cognitive impairment associated with schizophrenia. Schizophrenia is characterized by abnormalities in glutamatergic pathways related to NMDA receptor hypofunction. Inhibition of GlyT1 on the presynaptic membrane or astrocytes is hypothesized to increase glycine levels within the synapse. The NMDA receptor function may be enhanced by increasing levels of its co-agonist, glycine, within the synaptic cleft, which may lead to improvements in cognitive function.
KarXT is an investigational oral dual-drug fixed-dose combination of xanomeline and trospium. It is undergoing a phase 3 clinical trial for the treatment of schizophrenia. Xanomeline is a functionally preferring muscarinic M4 and M1 receptor agonist that readily passes into the central nervous system (CNS) to stimulate these receptors in key areas of the brain. Trospium is a non-selective muscarinic antagonist that does not cross into the CNS and reduces peripheral cholinergic side effects associated with xanomeline.