The olfactory nerve, also known as the first cranial nerve, cranial nerve I, or simply CN I, is a cranial nerve that contains sensory nerve fibers relating to the sense of smell.

The salivary glands in many vertebrates including mammals are exocrine glands that produce saliva through a system of ducts. Humans have three paired major salivary glands, as well as hundreds of minor salivary glands. Salivary glands can be classified as serous, mucous, or seromucous (mixed).

The vomeronasal organ (VNO), or Jacobson's organ, is the paired auxiliary olfactory (smell) sense organ located in the soft tissue of the nasal septum, in the nasal cavity just above the roof of the mouth in various tetrapods. The name is derived from the fact that it lies adjacent to the unpaired vomer bone in the nasal septum. It is present and functional in all snakes and lizards, and in many mammals, including cats, dogs, cattle, pigs, and some primates. Some humans may have physical remnants of a VNO, but it is vestigial and non-functional.

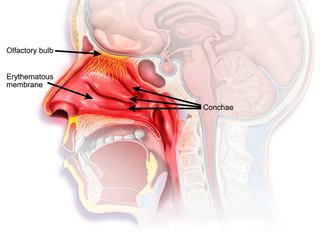
The nasal cavity is a large, air-filled space above and behind the nose in the middle of the face. The nasal septum divides the cavity into two cavities, also known as fossae. Each cavity is the continuation of one of the two nostrils. The nasal cavity is the uppermost part of the respiratory system and provides the nasal passage for inhaled air from the nostrils to the nasopharynx and rest of the respiratory tract.

The lamina propria is a thin layer of connective tissue that forms part of the moist linings known as mucous membranes or mucosae, which line various tubes in the body, such as the respiratory tract, the gastrointestinal tract, and the urogenital tract.

Immunoglobulin A is an antibody that plays a role in the immune function of mucous membranes. The amount of IgA produced in association with mucosal membranes is greater than all other types of antibody combined. In absolute terms, between three and five grams are secreted into the intestinal lumen each day. This represents up to 15% of total immunoglobulins produced throughout the body.

In physiology, a stimulus is a detectable change in the physical or chemical structure of an organism's internal or external environment. The ability of an organism or organ to detect external stimuli, so that an appropriate reaction can be made, is called sensitivity (excitability). Sensory receptors can receive information from outside the body, as in touch receptors found in the skin or light receptors in the eye, as well as from inside the body, as in chemoreceptors and mechanoreceptors. When a stimulus is detected by a sensory receptor, it can elicit a reflex via stimulus transduction. An internal stimulus is often the first component of a homeostatic control system. External stimuli are capable of producing systemic responses throughout the body, as in the fight-or-flight response. In order for a stimulus to be detected with high probability, its level of strength must exceed the absolute threshold; if a signal does reach threshold, the information is transmitted to the central nervous system (CNS), where it is integrated and a decision on how to react is made. Although stimuli commonly cause the body to respond, it is the CNS that finally determines whether a signal causes a reaction or not.

The olfactory epithelium is a specialized epithelial tissue inside the nasal cavity that is involved in smell. In humans, it measures 5 cm2 (0.78 sq in) and lies on the roof of the nasal cavity about 7 cm (2.8 in) above and behind the nostrils. The olfactory epithelium is the part of the olfactory system directly responsible for detecting odors.
The olfactory mucosa is the neuroepithelial mucosa lining the roof and upper parts of the septum and lateral wall of the nasal cavity which contains bipolar neurons of the primary receptor neurons of the olfactory pathway, as well as supporting cells. The neurons' dendrites project towards the nasal cavity while their axons ascend through the cribriform plate as the olfactory nerves.

Olfactory receptors (ORs), also known as odorant receptors, are chemoreceptors expressed in the cell membranes of olfactory receptor neurons and are responsible for the detection of odorants which give rise to the sense of smell. Activated olfactory receptors trigger nerve impulses which transmit information about odor to the brain. In vertebrates, these receptors are members of the class A rhodopsin-like family of G protein-coupled receptors (GPCRs). The olfactory receptors form the largest multigene family in vertebrates consisting of around 400 genes in humans and 1400 genes in mice. In insects, olfactory receptors are members of an unrelated group of ligand-gated ion channels.

Enterochromaffin (EC) cells are a type of enteroendocrine cell, and neuroendocrine cell. They reside alongside the epithelium lining the lumen of the digestive tract and play a crucial role in gastrointestinal regulation, particularly intestinal motility and secretion. They were discovered by Nikolai Kulchitsky.

A sustentacular cell is a type of cell primarily associated with structural support, they can be found in various tissues.
Gut-associated lymphoid tissue (GALT) is a component of the mucosa-associated lymphoid tissue (MALT) which works in the immune system to protect the body from invasion in the gut.

The gastric mucosa is the mucous membrane layer of the stomach, which contains the gastric pits, to which the gastric glands empty. In humans, it is about one mm thick, and its surface is smooth, soft, and velvety. It consists of simple secretory columnar epithelium, an underlying supportive layer of loose connective tissue called the lamina propria, and the muscularis mucosae, a thin layer of muscle that separates the mucosa from the underlying submucosa.
Dysosmia is a disorder described as any qualitative alteration or distortion of the perception of smell. Qualitative alterations differ from quantitative alterations, which include anosmia and hyposmia. Dysosmia can be classified as either parosmia or phantosmia. Parosmia is a distortion in the perception of an odorant. Odorants smell different from what one remembers. Phantosmia is the perception of an odor when no odorant is present. The cause of dysosmia still remains a theory. It is typically considered a neurological disorder and clinical associations with the disorder have been made. Most cases are described as idiopathic and the main antecedents related to parosmia are URTIs, head trauma, and nasal and paranasal sinus disease. Dysosmia tends to go away on its own but there are options for treatment for patients that want immediate relief.

The sense of smell, or olfaction, is the special sense through which smells are perceived. The sense of smell has many functions, including detecting desirable foods, hazards, and pheromones, and plays a role in taste.
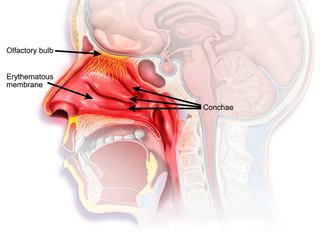
The nasal mucosa lines the nasal cavity. It is part of the respiratory mucosa, the mucous membrane lining the respiratory tract. The nasal mucosa is intimately adherent to the periosteum or perichondrium of the nasal conchae. It is continuous with the skin through the nostrils, and with the mucous membrane of the nasal part of the pharynx through the choanae. From the nasal cavity its continuity with the conjunctiva may be traced, through the nasolacrimal and lacrimal ducts; and with the frontal, ethmoidal, sphenoidal, and maxillary sinuses, through the several openings in the nasal meatuses. The mucous membrane is thickest, and most vascular, over the nasal conchae. It is also thick over the nasal septum where increased numbers of goblet cells produce a greater amount of nasal mucus. It is very thin in the meatuses on the floor of the nasal cavities, and in the various sinuses. It is one of the most commonly infected tissues in adults and children. Inflammation of this tissue may cause significant impairment of daily activities, with symptoms such as stuffy nose, headache, mouth breathing, etc.

The gastrointestinal wall of the gastrointestinal tract is made up of four layers of specialised tissue. From the inner cavity of the gut outwards, these are the mucosa, the submucosa, the muscular layer and the serosa or adventitia.

The intestinal mucosal barrier, also referred to as intestinal barrier, refers to the property of the intestinal mucosa that ensures adequate containment of undesirable luminal contents within the intestine while preserving the ability to absorb nutrients. The separation it provides between the body and the gut prevents the uncontrolled translocation of luminal contents into the body proper. Its role in protecting the mucosal tissues and circulatory system from exposure to pro-inflammatory molecules, such as microorganisms, toxins, and antigens is vital for the maintenance of health and well-being. Intestinal mucosal barrier dysfunction has been implicated in numerous health conditions such as: food allergies, microbial infections, irritable bowel syndrome, inflammatory bowel disease, celiac disease, metabolic syndrome, non-alcoholic fatty liver disease, diabetes, and septic shock.

BPI fold containing family B, member 3 (BPIFB3) is a protein that in humans is encoded by the BPIFB3 gene. Two variants have been detected in humans.