Related Research Articles

Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered state of consciousness due to ischemia in the brain.

Bronchiectasis is a disease in which there is permanent enlargement of parts of the airways of the lung. Symptoms typically include a chronic cough with mucus production. Other symptoms include shortness of breath, coughing up blood, and chest pain. Wheezing and nail clubbing may also occur. Those with the disease often get lung infections.

Pulmonary hypertension is a condition of increased blood pressure in the arteries of the lungs. Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise. Onset is typically gradual. According to the definition at the 6th World Symposium of Pulmonary Hypertension in 2018, a patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 20mmHg at rest, revised down from a purely arbitrary 25mmHg, and pulmonary vascular resistance (PVR) greater than 3 Wood units.
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation. While there are similarities with regard to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.

Chest physiotherapy (CPT) are treatments generally performed by physical therapists and respiratory therapists, whereby breathing is improved by the indirect removal of mucus from the breathing passages of a patient. Other terms include respiratory or cardio-thoracic physiotherapy.
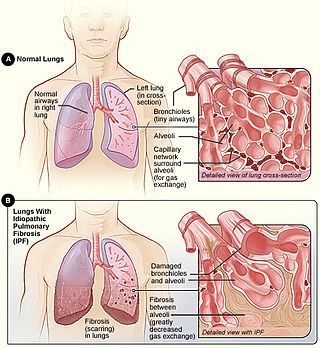
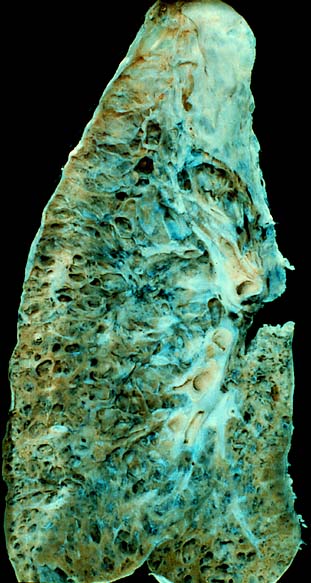
Idiopathic pulmonary fibrosis (IPF) synonymous with cryptogenic fibrosing alveolitis is a rare, progressive illness of the respiratory system, characterized by the thickening and stiffening of lung tissue, associated with the formation of scar tissue. It is a type of chronic pulmonary fibrosis characterized by a progressive and irreversible decline in lung function.

Erdosteine is a molecule with mucolytic activity. Structurally it is a thiol derivative characterized by the presence of two thiol groups. These two functional sulfhydryl groups contained in the molecule are released following first-pass metabolism with the conversion of erdosteine into its pharmacologically active metabolite Met-I.
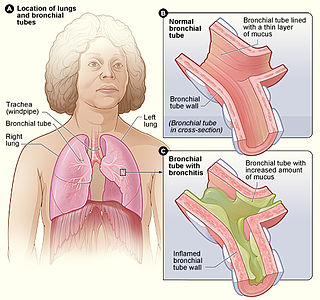
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.

Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a pulmonary function technologist, respiratory therapist, respiratory physiologist, physiotherapist, pulmonologist, or general practitioner.

The FEV1/FVC ratio, also called modified Tiffeneau-Pinelli index, is a calculated ratio used in the diagnosis of obstructive and restrictive lung disease. It represents the proportion of a person's vital capacity that they are able to expire in the first second of forced expiration (FEV1) to the full, forced vital capacity (FVC). FEV1/FVC ratio was first proposed by E.A. Haensler in 1950. The FEV1/FVC index should not be confused with the FEV1/VC index as they are different, although both are intended for diagnosing airway obstruction. Current recommendations for diagnosing pulmonary function recommend using the modified Tiffeneau-Pinelli index. This index is recommended to be represented as a decimal fraction with two digits after the decimal point.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.
In some individuals, the effect of oxygen on chronic obstructive pulmonary disease is to cause increased carbon dioxide retention,

Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms due to abnormalities of the airways and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.
Physiotherapists treating patients following uncomplicated coronary artery bypass surgery surgery continue to use interventions such as deep breathing exercises that are not supported by best available evidence. Standardised guidelines may be required to better match clinical practice with current literature.

Emphysema is any air-filled enlargement in the body's tissues. Most commonly emphysema refers to the permanent enlargement of air spaces (alveoli) in the lungs, and is also known as pulmonary emphysema.
Jadwiga “Wisia” A. Wedzicha is a British physician and Professor of Respiratory Medicine at the National Heart and Lung Institute. Her research has considered the causes and impact of chronic obstructive pulmonary disease. She was elected as Fellow of the UK Academy of Medical Sciences in 2013 and awarded the Helmholtz International Fellow Award.
References
- 1 2 Sweeney G. "Pulmonary Rehabilitation" . Retrieved 8 June 2011.
- ↑ Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. (June 2006). "American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation". American Journal of Respiratory and Critical Care Medicine. 173 (12): 1390–1413. doi:10.1164/rccm.200508-1211ST. PMID 16760357.
- ↑ Sharma S, Arneja A, Massagli TL. Talavera F, Salcido R, Kishner S (eds.). "Pulmonary Rehabilitation". eMedicine. Retrieved 8 June 2011.
- 1 2 3 "Pulmonary Rehabilitation". AARC Clinical Practice Guideline. Respiratory Care . Retrieved 8 June 2011.
- 1 2 3 "CG101 Chronic obstructive pulmonary disease (update): full guideline" (PDF). National Clinical Guideline Centre. Royal College of Physicians of London. 2004. Archived from the original (PDF) on 5 September 2012.
- ↑ Kalamara EI, Ballas ET, Pitsiou G, Petrova G (March 2021). "Pulmonary rehabilitation for cystic fibrosis: A narrative review of current literature". Monaldi Archives for Chest Disease = Archivio Monaldi per le Malattie del Torace. 91 (2). doi: 10.4081/monaldi.2021.1501 . PMID 33792230. S2CID 232481541.
- ↑ Guber E, Wand O, Epstein Shochet G, Romem A, Shitrit D (2021-03-30). "The Short- and Long-Term Impact of Pulmonary Rehabilitation in Subjects with Sarcoidosis: A Prospective Study and Review of the Literature". Respiration; International Review of Thoracic Diseases. 100 (5): 423–431. doi:10.1159/000514917. PMID 33784708. S2CID 232432025.
- 1 2 Dowman L, Hill CJ, May A, Holland AE (February 2021). "Pulmonary rehabilitation for interstitial lung disease". The Cochrane Database of Systematic Reviews. 2021 (2): CD006322. doi:10.1002/14651858.CD006322.pub4. PMC 8094410 . PMID 34559419.
- 1 2 3 Şahin H, Naz İ, Aksel N, Güldaval F, Gayaf M, Yazgan S, Ceylan KC (April 2022). "Outcomes of pulmonary rehabilitation after lung resection in patients with lung cancer". Turk Gogus Kalp Damar Cerrahisi Dergisi. 30 (2): 227–234. doi:10.5606/tgkdc.dergisi.2022.21595. PMC 9473605 . PMID 36168581.
- ↑ Osadnik CR, Gleeson C, McDonald VM, Holland AE, et al. (Cochrane Airways Group) (August 2022). "Pulmonary rehabilitation versus usual care for adults with asthma". The Cochrane Database of Systematic Reviews. 2022 (8): CD013485. doi:10.1002/14651858.CD013485.pub2. PMC 9394585 . PMID 35993916.
- ↑ Hume E, Ward L, Wilkinson M, Manifield J, Clark S, Vogiatzis I (December 2020). "Exercise training for lung transplant candidates and recipients: a systematic review". European Respiratory Review. 29 (158): 200053. doi:10.1183/16000617.0053-2020. PMC 9488968 . PMID 33115788.
- ↑ Morris NR, Kermeen FD, Jones AW, Lee JY, Holland AE, et al. (Cochrane Airways Group) (March 2023). "Exercise-based rehabilitation programmes for pulmonary hypertension". The Cochrane Database of Systematic Reviews. 2023 (3): CD011285. doi:10.1002/14651858.CD011285.pub3. PMC 10032353 . PMID 36947725.
- ↑ Griffiths TL, Phillips CJ, Davies S, Burr ML, Campbell IA (October 2001). "Cost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programme". Thorax. 56 (10): 779–784. doi:10.1136/thorax.56.10.779. PMC 1745931 . PMID 11562517.
- ↑ Güell R, Casan P, Belda J, Sangenis M, Morante F, Guyatt GH, Sanchis J (April 2000). "Long-term effects of outpatient rehabilitation of COPD: A randomized trial". Chest. 117 (4): 976–983. doi:10.1378/chest.117.4.976. PMID 10767227.
- ↑ Foglio K, Bianchi L, Bruletti G, Battista L, Pagani M, Ambrosino N (January 1999). "Long-term effectiveness of pulmonary rehabilitation in patients with chronic airway obstruction". The European Respiratory Journal. 13 (1): 125–132. doi: 10.1183/09031936.99.13112599 . PMID 10836336.
- 1 2 3 Killian KJ, Leblanc P, Martin DH, Summers E, Jones NL, Campbell EJ (October 1992). "Exercise capacity and ventilatory, circulatory, and symptom limitation in patients with chronic airflow limitation". The American Review of Respiratory Disease. 146 (4): 935–940. doi:10.1164/ajrccm/146.4.935. PMID 1416421.
- 1 2 Bernard S, LeBlanc P, Whittom F, Carrier G, Jobin J, Belleau R, Maltais F (August 1998). "Peripheral muscle weakness in patients with chronic obstructive pulmonary disease". American Journal of Respiratory and Critical Care Medicine. 158 (2): 629–634. doi:10.1164/ajrccm.158.2.9711023. PMID 9700144.
- ↑ Ries AL, Bauldoff GS, Carlin BW, Casaburi R, Emery CF, Mahler DA, et al. (May 2007). "Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines". Chest. 131 (5 Suppl): 4S–42S. doi: 10.1378/chest.06-2418 . PMID 17494825.
- ↑ British Thoracic Society Standards of Care Subcommittee on Pulmonary Rehabilitation (November 2001). "Pulmonary rehabilitation". Thorax. 56 (11): 827–834. doi:10.1136/thorax.56.11.827. PMC 1745955 . PMID 11641505.
- ↑ Marciniuk DD, Brooks D, Butcher S, Debigare R, Dechman G, Ford G, et al. (2010). "Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease--practical issues: a Canadian Thoracic Society Clinical Practice Guideline". Canadian Respiratory Journal. 17 (4): 159–168. doi: 10.1155/2010/425975 . PMC 2933771 . PMID 20808973. Archived from the original on 7 December 2010.
- ↑ "Pulmonary rehabilitation service for patients with COPD" (PDF). The National Institute for Health and Care Excellence (NICE). the National Health Service (NHS). December 2006. Archived from the original (PDF) on 4 May 2011.
- ↑ "Pulmonary rehabilitation". The National Institute for Health and Care Excellence (NICE). Archived from the original on 2 May 2012.
- ↑ Bhatt S. "Cardio-Pulmonary Rehab". University of Alabama Medicine. Retrieved 19 November 2017.
- ↑ Jones PW, Harding G, Wiklund I, Berry P, Tabberer M, Yu R, Leidy NK (July 2012). "Tests of the responsiveness of the COPD assessment test following acute exacerbation and pulmonary rehabilitation". Chest. 142 (1): 134–140. doi:10.1378/chest.11-0309. PMID 22281796.