Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

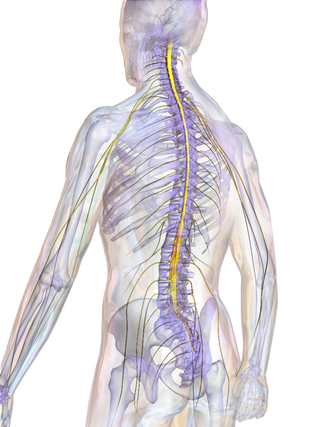
The cauda equina is a bundle of spinal nerves and spinal nerve rootlets, consisting of the second through fifth lumbar nerve pairs, the first through fifth sacral nerve pairs, and the coccygeal nerve, all of which arise from the lumbar enlargement and the conus medullaris of the spinal cord. The cauda equina occupies the lumbar cistern, a subarachnoid space inferior to the conus medullaris. The nerves that compose the cauda equina innervate the pelvic organs and lower limbs to include motor innervation of the hips, knees, ankles, feet, internal anal sphincter and external anal sphincter. In addition, the cauda equina extends to sensory innervation of the perineum and, partially, parasympathetic innervation of the bladder.
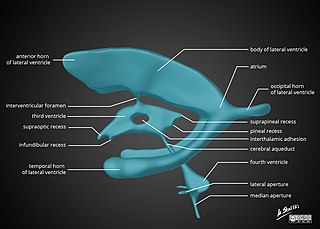
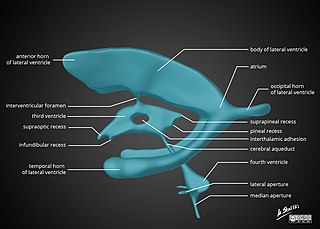
In neuroanatomy, the ventricular system is a set of four interconnected cavities known as cerebral ventricles in the brain. Within each ventricle is a region of choroid plexus which produces the circulating cerebrospinal fluid (CSF). The ventricular system is continuous with the central canal of the spinal cord from the fourth ventricle, allowing for the flow of CSF to circulate.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.

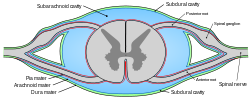
In anatomy, the meninges are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in the subarachnoid space between the arachnoid mater and the pia mater. The primary function of the meninges is to protect the central nervous system.

The dura mater, is the outermost of the three meningeal membranes. The dura mater has two layers, an outer periosteal layer closely adhered to the neurocranium, and an inner meningeal layer known as the dural border cell layer. The two dural layers are for the most part fused together forming a thick fibrous tissue membrane that covers the brain and the vertebrae of the spinal column. But the layers are separated at the dural venous sinuses to allow blood to drain from the brain. The dura covers the arachnoid mater and the pia mater the other two meninges in protecting the central nervous system.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true anaesthesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Combined spinal and epidural anaesthesia is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block. The indwelling epidural catheter gives the ability to provide long lasting analgesia and to titrate the dose given to the desired effect.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

In anatomy, the epidural space is the potential space between the dura mater and vertebrae (spine).

Neuromeres are distinct groups of neural crest cells, forming segments in the neural tube of the early embryonic development of the brain. There are three classes of neuromeres in the central nervous system – prosomeres, mesomeres and rhombomeres that will develop the forebrain, midbrain, and hindbrain respectively.

The filum terminale is a delicate strand of fibrous tissue, about 20 cm in length, extending inferiorly from the apex of the conus medullaris to attach onto the coccyx. The filum terminale acts to anchor the spinal cord and spinal meninges inferiorly.

The arachnoid mater is one of the three meninges, the protective membranes that cover the brain and spinal cord. It is so named because of its resemblance to a spider web. The arachnoid mater is a derivative of the neural crest mesoectoderm in the embryo.

Myelography is a type of radiographic examination that uses a contrast medium to detect pathology of the spinal cord, including the location of a spinal cord injury, cysts, and tumors. Historically the procedure involved the injection of a radiocontrast agent into the cervical or lumbar spine, followed by several X-ray projections. Today, myelography has largely been replaced by the use of MRI scans, although the technique is still sometimes used under certain circumstances – though now usually in conjunction with CT rather than X-ray projections.

In neurology, diastematomyelia is a congenital disorder in which a part of the spinal cord is split, usually at the level of the upper lumbar vertebra in the longitudinal (sagittal) direction. Females are affected much more commonly than males. This condition occurs in the presence of an osseous, cartilaginous or fibrous septum in the central portion of the spinal canal which then produces a complete or incomplete sagittal division of the spinal cord into two hemicords. When the split does not reunite distally to the spur, the condition is referred to as diplomyelia, which is true duplication of the spinal cord.

Post-dural-puncture headache (PDPH) is a complication of puncture of the dura mater. The headache is severe and described as "searing and spreading like hot metal", involving the back and front of the head and spreading to the neck and shoulders, sometimes involving neck stiffness. It is exacerbated by movement and sitting or standing and is relieved to some degree by lying down. Nausea, vomiting, pain in arms and legs, hearing loss, tinnitus, vertigo, dizziness and paraesthesia of the scalp are also common.

An epidural blood patch (EBP) is a surgical procedure that uses autologous blood, meaning the patient's own blood, in order to close one or many holes in the dura mater of the spinal cord, which occurred as a complication of a lumbar puncture or epidural placement. The punctured dura causes cerebrospinal fluid leak. The procedure can be used to relieve orthostatic headaches, most commonly post dural puncture headache (PDPH).
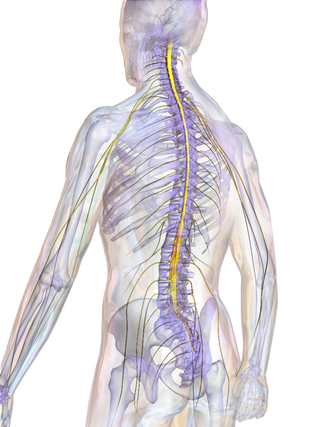
The spinal cord is a long, thin, tubular structure made up of nervous tissue that extends from the medulla oblongata in the lower brainstem to the lumbar region of the vertebral column (backbone) of vertebrate animals. The center of the spinal cord is hollow and contains a structure called the central canal, which contains cerebrospinal fluid. The spinal cord is also covered by meninges and enclosed by the neural arches. Together, the brain and spinal cord make up the central nervous system.

A cerebrospinal fluid leak is a medical condition where the cerebrospinal fluid (CSF) that surrounds the brain and spinal cord leaks out of one or more holes or tears in the dura mater. A CSF leak is classed as either spontaneous (primary), having no known cause, or nonspontaneous (secondary) where it is attributed to an underlying condition. Causes of a primary CSF leak are those of trauma including from an accident or intentional injury, or arising from a medical intervention known as iatrogenic. A basilar skull fracture as a cause can give the sign of CSF leakage from the ear, nose or mouth. A lumbar puncture can give the symptom of a post-dural-puncture headache.

Tarlov cysts, are type II innervated meningeal cysts, cerebrospinal-fluid-filled (CSF) sacs most frequently located in the spinal canal of the sacral region of the spinal cord (S1–S5) and much less often in the cervical, thoracic or lumbar spine. They can be distinguished from other meningeal cysts by their nerve-fiber-filled walls. Tarlov cysts are defined as cysts formed within the nerve-root sheath at the dorsal root ganglion. The etiology of these cysts is not well understood; some current theories explaining this phenomenon have not yet been tested or challenged but include increased pressure in CSF, filling of congenital cysts with one-way valves, and/or inflammation in response to trauma and disease. They are named for American neurosurgeon Isadore Tarlov, who described them in 1938.