Tetraplegia, also known as quadriplegia, is defined as the dysfunction or loss of motor and/or sensory function in the cervical area of the spinal cord. A loss of motor function can present as either weakness or paralysis leading to partial or total loss of function in the arms, legs, trunk, and pelvis. The paralysis may be flaccid or spastic. A loss of sensory function can present as an impairment or complete inability to sense light touch, pressure, heat, pinprick/pain, and proprioception. In these types of spinal cord injury, it is common to have a loss of both sensation and motor control.

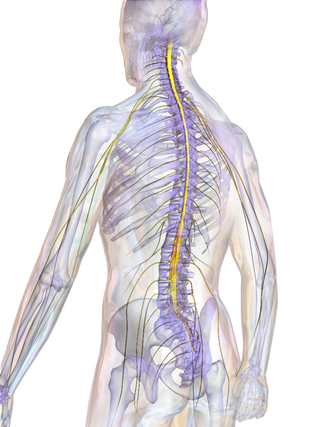
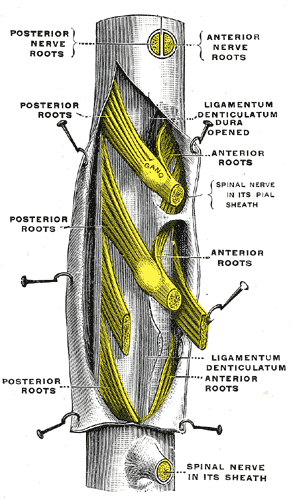
A spinal nerve is a mixed nerve, which carries motor, sensory, and autonomic signals between the spinal cord and the body. In the human body there are 31 pairs of spinal nerves, one on each side of the vertebral column. These are grouped into the corresponding cervical, thoracic, lumbar, sacral and coccygeal regions of the spine. There are eight pairs of cervical nerves, twelve pairs of thoracic nerves, five pairs of lumbar nerves, five pairs of sacral nerves, and one pair of coccygeal nerves. The spinal nerves are part of the peripheral nervous system.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.

Sciatica is pain going down the leg from the lower back. This pain may go down the back, outside, or front of the leg. Onset is often sudden following activities such as heavy lifting, though gradual onset may also occur. The pain is often described as shooting. Typically, symptoms are only on one side of the body. Certain causes, however, may result in pain on both sides. Lower back pain is sometimes present. Weakness or numbness may occur in various parts of the affected leg and foot.
The ankle jerk reflex, also known as the Achilles reflex, occurs when the Achilles tendon is tapped while the foot is dorsiflexed. It is a type of stretch reflex that tests the function of the gastrocnemius muscle and the nerve that supplies it. A positive result would be the jerking of the foot towards its plantar surface. Being a deep tendon reflex, it is monosynaptic. It is also a stretch reflex. These are monosynaptic spinal segmental reflexes. When they are intact, integrity of the following is confirmed: cutaneous innervation, motor supply, and cortical input to the corresponding spinal segment.

In tetrapod anatomy, lumbar is an adjective that means of or pertaining to the abdominal segment of the torso, between the diaphragm and the sacrum.

A discectomy is the surgical removal of abnormal disc material that presses on a nerve root or the spinal cord. The procedure involves removing a portion of an intervertebral disc, which causes pain, weakness or numbness by stressing the spinal cord or radiating nerves. The traditional open discectomy, or Love's technique, was published by Ross and Love in 1971. Advances have produced visualization improvements to traditional discectomy procedures, or endoscopic discectomy. In conjunction with the traditional discectomy or microdiscectomy, a laminotomy is often involved to permit access to the intervertebral disc. Laminotomy means a significant amount of typically normal bone is removed from the vertebra, allowing the surgeon to better see and access the area of disc herniation.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true anaesthesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

Neuromeres are distinct groups of neural crest cells, forming segments in the neural tube of the early embryonic development of the brain. There are three classes of neuromeres in the central nervous system – prosomeres, mesomeres and rhombomeres that will develop the forebrain, midbrain, and hindbrain respectively.

Cauda equina syndrome (CES) is a condition that occurs when the bundle of nerves below the end of the spinal cord known as the cauda equina is damaged. Signs and symptoms include low back pain, pain that radiates down the leg, numbness around the anus, and loss of bowel or bladder control. Onset may be rapid or gradual.
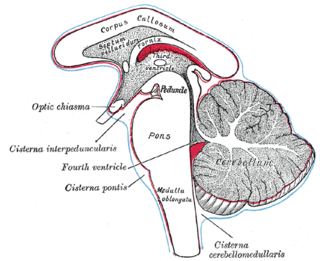
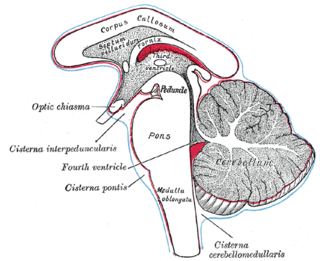
The subarachnoid cisterns are spaces formed by openings in the subarachnoid space, an anatomic space in the meninges of the brain. The space is situated between the two meninges, the arachnoid mater and the pia mater. These cisterns are filled with cerebrospinal fluid (CSF).

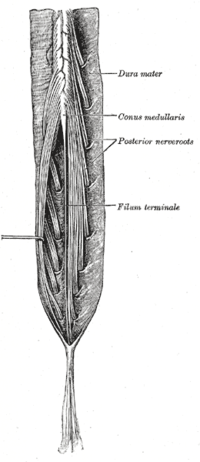
The conus medullaris or conus terminalis is the tapered, lower end of the spinal cord. It occurs near lumbar vertebral levels 1 (L1) and 2 (L2), occasionally lower. The upper end of the conus medullaris is usually not well defined, however, its corresponding spinal cord segments are usually S1–S5.

Myelography is a type of radiographic examination that uses a contrast medium to detect pathology of the spinal cord, including the location of a spinal cord injury, cysts, and tumors. Historically the procedure involved the injection of a radiocontrast agent into the cervical or lumbar spine, followed by several X-ray projections. Today, myelography has largely been replaced by the use of MRI scans, although the technique is still sometimes used under certain circumstances – though now usually in conjunction with CT rather than X-ray projections.

A disc herniation or spinal disc herniation is an injury to the intervertebral disc between two vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatments may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including good posture.
Tethered cord syndrome (TCS) refers to a group of neurological disorders that relate to malformations of the spinal cord. Various forms include tight filum terminale, lipomeningomyelocele, split cord malformations (diastematomyelia), occult, dermal sinus tracts, and dermoids. All forms involve the pulling of the spinal cord at the base of the spinal canal, literally a tethered cord. The spinal cord normally hangs loose in the canal, free to move up and down with growth, and with bending and stretching. A tethered cord, however, is held taut at the end or at some point in the spinal canal. In children, a tethered cord can force the spinal cord to stretch as they grow. In adults the spinal cord stretches in the course of normal activity, usually leading to progressive spinal cord damage if untreated. TCS is often associated with the closure of a spina bifida. It can be congenital, such as in tight filum terminale, or the result of injury later in life.
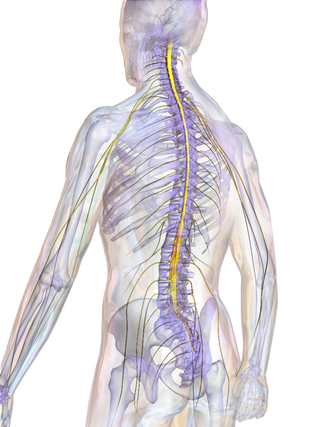
The spinal cord is a long, thin, tubular structure made up of nervous tissue that extends from the medulla oblongata in the lower brainstem to the lumbar region of the vertebral column (backbone) of vertebrate animals. The center of the spinal cord is hollow and contains a structure called the central canal, which contains cerebrospinal fluid. The spinal cord is also covered by meninges and enclosed by the neural arches. Together, the brain and spinal cord make up the central nervous system.

Spinal disease refers to a condition impairing the backbone. These include various diseases of the back or spine ("dorso-"), such as kyphosis. Dorsalgia refers to back pain. Some other spinal diseases include spinal muscular atrophy, ankylosing spondylitis, scoliosis, lumbar spinal stenosis, spina bifida, spinal tumors, osteoporosis and cauda equina syndrome.
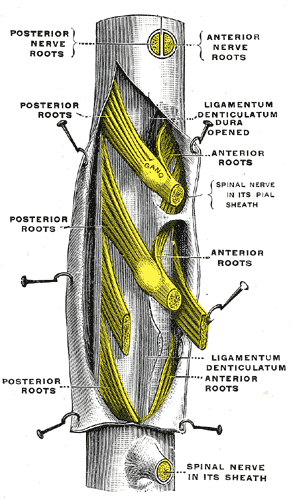
The thecal sac or dural sac is the membranous sheath (theca) or tube of dura mater that surrounds the spinal cord and the cauda equina. The thecal sac contains the cerebrospinal fluid which provides nutrients and buoyancy to the spinal cord. From the skull the tube adheres to bone at the foramen magnum and extends down to the second sacral vertebra where it tapers to cover over the filum terminale. Along most of the spinal canal it is separated from the inner surface by the epidural space. The sac has projections that follow the spinal nerves along their paths out of the vertebral canal which become the dural root sheaths.

A spinal fracture, also called a vertebral fracture or a broken back, is a fracture affecting the vertebrae of the spinal column. Most types of spinal fracture confer a significant risk of spinal cord injury. After the immediate trauma, there is a risk of spinal cord injury if the fracture is unstable, that is, likely to change alignment without internal or external fixation.

Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with leaning forward. Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.