The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about 12 centimetres in length. They receive blood from the paired renal arteries; blood exits into the paired renal veins. Each kidney is attached to a ureter, a tube that carries excreted urine to the bladder.

The urinary system, also known as the urinary tract or renal system, consists of the kidneys, ureters, bladder, and the urethra. The purpose of the urinary system is to eliminate waste from the body, regulate blood volume and blood pressure, control levels of electrolytes and metabolites, and regulate blood pH. The urinary tract is the body's drainage system for the eventual removal of urine. The kidneys have an extensive blood supply via the renal arteries which leave the kidneys via the renal vein. Each kidney consists of functional units called nephrons. Following filtration of blood and further processing, wastes exit the kidney via the ureters, tubes made of smooth muscle fibres that propel urine towards the urinary bladder, where it is stored and subsequently expelled from the body by urination (voiding). The female and male urinary system are very similar, differing only in the length of the urethra.
Albuminuria is a pathological condition wherein the protein albumin is abnormally present in the urine. It is a type of proteinuria. Albumin is a major plasma protein ; in healthy people, only trace amounts of it are present in urine, whereas larger amounts occur in the urine of patients with kidney disease. For a number of reasons, clinical terminology is changing to focus on albuminuria more than proteinuria.

Proteinuria is the presence of excess proteins in the urine. In healthy persons, urine contains very little protein; an excess is suggestive of illness. Excess protein in the urine often causes the urine to become foamy. Severe proteinuria can cause nephrotic syndrome in which there is worsening swelling of the body.
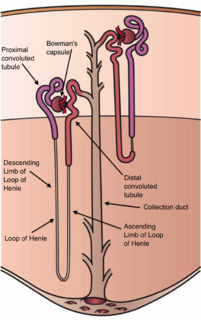
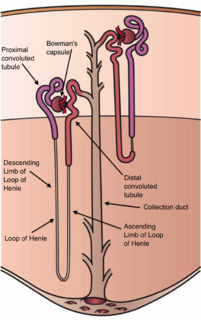
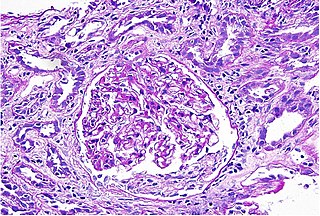
The nephron is the minute or microscopic structural and functional unit of the kidney. It is composed of a renal corpuscle and a renal tubule. The renal corpuscle consists of a tuft of capillaries called a glomerulus and a cup-shaped structure called Bowman's capsule. The renal tubule extends from the capsule. The capsule and tubule are connected and are composed of epithelial cells with a lumen. A healthy adult has 1 to 1.5 million nephrons in each kidney. Blood is filtered as it passes through three layers: the endothelial cells of the capillary wall, its basement membrane, and between the foot processes of the podocytes of the lining of the capsule. The tubule has adjacent peritubular capillaries that run between the descending and ascending portions of the tubule. As the fluid from the capsule flows down into the tubule, it is processed by the epithelial cells lining the tubule: water is reabsorbed and substances are exchanged ; first with the interstitial fluid outside the tubules, and then into the plasma in the adjacent peritubular capillaries through the endothelial cells lining that capillary. This process regulates the volume of body fluid as well as levels of many body substances. At the end of the tubule, the remaining fluid—urine—exits: it is composed of water, metabolic waste, and toxins.

Nephrotic syndrome is a collection of symptoms due to kidney damage. This includes protein in the urine, low blood albumin levels, high blood lipids, and significant swelling. Other symptoms may include weight gain, feeling tired, and foamy urine. Complications may include blood clots, infections, and high blood pressure.

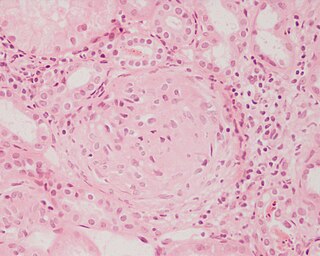
Nephritis is inflammation of the kidneys and may involve the glomeruli, tubules, or interstitial tissue surrounding the glomeruli and tubules. It is one of several different types of nephropathy.

The proximal tubule is the segment of the nephron in kidneys which begins from the renal pole of the Bowman's capsule to the beginning of loop of Henle. It can be further classified into the proximal convoluted tubule (PCT) and the proximal straight tubule (PST).

Urinalysis, a portmanteau of the words urine and analysis, is a panel of medical tests that includes physical (macroscopic) examination of the urine, chemical evaluation using urine test strips, and microscopic examination. Macroscopic examination targets parameters such as color, clarity, odor, and specific gravity; urine test strips measure chemical properties such as pH, glucose concentration, and protein levels; and microscopy is performed to identify elements such as cells, urinary casts, crystals, and organisms.
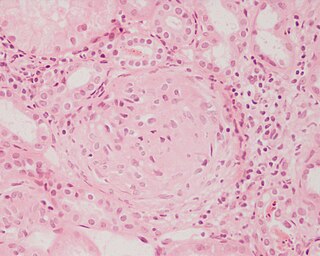
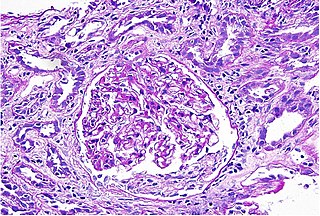
Glomerulonephritis (GN) is a term used to refer to several kidney diseases. Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the name, but not all diseases necessarily have an inflammatory component.
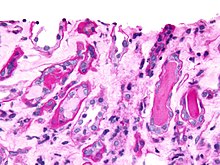
Acute tubular necrosis (ATN) is a medical condition involving the death of tubular epithelial cells that form the renal tubules of the kidneys. Because necrosis is often not present, the term acute tubular injury (ATI) is preferred by pathologists over the older name acute tubular necrosis (ATN). ATN presents with acute kidney injury (AKI) and is one of the most common causes of AKI. Common causes of ATN include low blood pressure and use of nephrotoxic drugs. The presence of "muddy brown casts" of epithelial cells found in the urine during urinalysis is pathognomonic for ATN. Management relies on aggressive treatment of the factors that precipitated ATN. Because the tubular cells continually replace themselves, the overall prognosis for ATN is quite good if the underlying cause is corrected, and recovery is likely within 7 to 21 days.

Minimal change disease is a disease affecting the kidneys which causes a nephrotic syndrome. Nephrotic syndrome leads to the loss of significant amounts of protein in the urine, which causes the widespread edema and impaired kidney function commonly experienced by those affected by the disease. It is most common in children and has a peak incidence at 2 to 6 years of age. MCD is responsible for 10–25% of nephrotic syndrome cases in adults. It is also the most common cause of nephrotic syndrome of unclear cause (idiopathic) in children.
Interstitial nephritis, also known as tubulointerstitial nephritis, is inflammation of the area of the kidney known as the renal interstitium, which consists of a collection of cells, extracellular matrix, and fluid surrounding the renal tubules. In addition to providing a scaffolding support for the tubular architecture, the interstitium has been shown to participate in the fluid and electrolyte exchange as well as endocrine functions of the kidney.
Acute uric acid nephropathy is a rapidly worsening (decreasing) kidney function that is caused by high levels of uric acid in the urine (hyperuricosuria).
Kidney development, or nephrogenesis, describes the embryologic origins of the kidney, a major organ in the urinary system. This article covers a 3 part developmental process that is observed in most reptiles, birds and mammals, including humans. Nephrogenesis is often considered in the broader context of the development of the urinary and reproductive organs.

Uromodulin (UMOD), also known as Tamm–Horsfall protein (THP), is a Zona pellucida-like domain-containing glycoprotein that in humans is encoded by the UMOD gene. Uromodulin is the most abundant protein excreted in ordinary urine.
Congenital nephrotic syndrome is a rare kidney disease which manifests in infants during the first 3 months of life, and is characterized by high levels of protein in the urine (proteinuria), low levels of protein in the blood, and swelling. This disease is primarily caused by genetic mutations which result in damage to components of the glomerular filtration barrier and allow for leakage of plasma proteins into the urinary space.

Within the nephron of the kidney, the ascending limb of the loop of Henle is a segment of the heterogenous loop of Henle downstream of the descending limb, after the sharp bend of the loop. This part of the renal tubule is divided into a thin and thick ascending limb; the thick portion is also known as the distal straight tubule, in contrast with the distal convoluted tubule downstream.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Glomerulonephrosis is a non-inflammatory disease of the kidney (nephrosis) presenting primarily in the glomerulus as Nephrotic Syndrome. The nephron is the functional unit of the kidney and it contains the glomerulus, which acts as a filter for blood to retain proteins and blood lipids. Damage to these filtration units results in important blood contents being released as waste in urine. This disease can be characterized by symptoms such as fatigue, swelling, and foamy urine, and can lead to chronic kidney disease and ultimately end-stage renal disease, as well as cardiovascular diseases. Glomerulonephrosis can present as either primary glomerulonephrosis or secondary glomerulonephrosis.