Bacillus Calmette–Guérin (BCG) vaccine is a vaccine primarily used against tuberculosis (TB). It is named after its inventors Albert Calmette and Camille Guérin. In countries where tuberculosis or leprosy is common, one dose is recommended in healthy babies as soon after birth as possible. In areas where tuberculosis is not common, only children at high risk are typically immunized, while suspected cases of tuberculosis are individually tested for and treated. Adults who do not have tuberculosis and have not been previously immunized, but are frequently exposed, may be immunized, as well. BCG also has some effectiveness against Buruli ulcer infection and other nontuberculous mycobacterial infections. Additionally, it is sometimes used as part of the treatment of bladder cancer.

Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating the body's adaptive immunity, they help prevent sickness from an infectious disease. When a sufficiently large percentage of a population has been vaccinated, herd immunity results. Herd immunity protects those who may be immunocompromised and cannot get a vaccine because even a weakened version would harm them. The effectiveness of vaccination has been widely studied and verified. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the elimination of diseases such as polio and tetanus from much of the world. However, some diseases, such as measles outbreaks in America, have seen rising cases due to relatively low vaccination rates in the 2010s – attributed, in part, to vaccine hesitancy. According to the World Health Organization, vaccination prevents 3.5–5 million deaths per year.

A vaccine is a biological preparation that provides active acquired immunity to a particular infectious or malignant disease. The safety and effectiveness of vaccines has been widely studied and verified. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins. The agent stimulates the body's immune system to recognize the agent as a threat, destroy it, and recognize further and destroy any of the microorganisms associated with that agent that it may encounter in the future.

Anthrax is an infection caused by the bacterium Bacillus anthracis. Infection typically occurs by contact with the skin, inhalation, or intestinal absorption. Symptom onset occurs between one day and more than two months after the infection is contracted. The skin form presents with a small blister with surrounding swelling that often turns into a painless ulcer with a black center. The inhalation form presents with fever, chest pain and shortness of breath. The intestinal form presents with diarrhea, abdominal pains, nausea and vomiting.

The smallpox vaccine is the first vaccine to have been developed against a contagious disease. In 1796, British physician Edward Jenner demonstrated that an infection with the relatively mild cowpox virus conferred immunity against the deadly smallpox virus. Cowpox served as a natural vaccine until the modern smallpox vaccine emerged in the 20th century. From 1958 to 1977, the World Health Organization (WHO) conducted a global vaccination campaign that eradicated smallpox, making it the only human disease to be eradicated. Although routine smallpox vaccination is no longer performed on the general public, the vaccine is still being produced to guard against bioterrorism, biological warfare, and mpox.

Immunization, or immunisation, is the process by which an individual's immune system becomes fortified against an infectious agent.
In biology, immunity is the state of being insusceptible or resistant to a noxious agent or process, especially a pathogen or infectious disease. Immunity may occur naturally or be produced by prior exposure or immunization.

Vaccinia virus is a large, complex, enveloped virus belonging to the poxvirus family. It has a linear, double-stranded DNA genome approximately 190 kbp in length, which encodes approximately 250 genes. The dimensions of the virion are roughly 360 × 270 × 250 nm, with a mass of approximately 5–10 fg. The vaccinia virus is the source of the modern smallpox vaccine, which the World Health Organization (WHO) used to eradicate smallpox in a global vaccination campaign in 1958–1977. Although smallpox no longer exists in the wild, vaccinia virus is still studied widely by scientists as a tool for gene therapy and genetic engineering.

Vaccine hesitancy is a delay in acceptance, or refusal, of vaccines despite the availability of vaccine services and supporting evidence. The term covers refusals to vaccinate, delaying vaccines, accepting vaccines but remaining uncertain about their use, or using certain vaccines but not others. The scientific consensus that vaccines are generally safe and effective is overwhelming. Vaccine hesitancy often results in disease outbreaks and deaths from vaccine-preventable diseases. Therefore, the World Health Organization characterizes vaccine hesitancy as one of the top ten global health threats.
The Ames strain is one of 89 known strains of the anthrax bacterium. It was isolated from a diseased 14-month-old Beefmaster heifer that died in Sarita, Texas in 1981. The strain was isolated at the Texas Veterinary Medical Diagnostic Laboratory and a sample was sent to the United States Army Medical Research Institute of Infectious Diseases (USAMRIID). Researchers at USAMRIID mistakenly believed the strain came from Ames, Iowa because the return address on the package was the USDA's National Veterinary Services Laboratories in Ames and mislabeled the specimen.
Artificial induction of immunity is immunization achieved by human efforts in preventive healthcare, as opposed to natural immunity as produced by organisms' immune systems. It makes people immune to specific diseases by means other than waiting for them to catch the disease. The purpose is to reduce the risk of death and suffering, that is, the disease burden, even when eradication of the disease is not possible. Vaccination is the chief type of such immunization, greatly reducing the burden of vaccine-preventable diseases.
Tuberculosis (TB) vaccines are vaccinations intended for the prevention of tuberculosis. Immunotherapy as a defence against TB was first proposed in 1890 by Robert Koch. Today, the only effective tuberculosis vaccine in common use is the Bacillus Calmette-Guérin (BCG) vaccine, first used on humans in 1921. It consists of attenuated (weakened) strains of the cattle tuberculosis bacillus. It is recommended for babies in countries where tuberculosis is common.

Mumps vaccines are vaccines which prevent mumps. When given to a majority of the population they decrease complications at the population level. Effectiveness when 90% of a population is vaccinated is estimated at 85%. Two doses are required for long term prevention. The initial dose is recommended between 12 and 18 months of age. The second dose is then typically given between two years and six years of age. Usage after exposure in those not already immune may be useful.
The Anthrax Vaccine Immunization Program (AVIP), is the name of the policy set forth by the U.S. federal government to immunize its military and certain civilian personnel with BioThrax, an anthrax vaccine manufactured by Emergent BioSolutions Inc. It was set up by the Clinton administration.
An attenuated vaccine is a vaccine created by reducing the virulence of a pathogen, but still keeping it viable. Attenuation takes an infectious agent and alters it so that it becomes harmless or less virulent. These vaccines contrast to those produced by "killing" the pathogen.
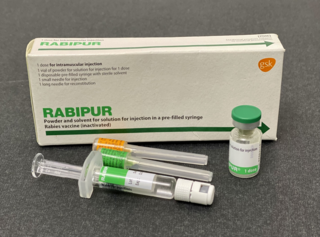
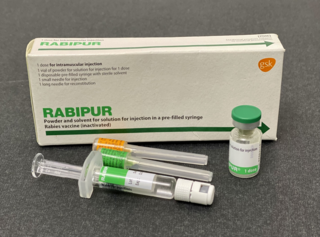
The rabies vaccine is a vaccine used to prevent rabies. There are several rabies vaccines available that are both safe and effective. Vaccinations must be administered prior to rabies virus exposure or within the latent period after exposure to prevent the disease. Transmission of rabies virus to humans typically occurs through a bite or scratch from an infectious animal, but exposure can occur through indirect contact with the saliva from an infectious individual.

Bacillus anthracis is a gram-positive and rod-shaped bacterium that causes anthrax, a deadly disease to livestock and, occasionally, to humans. It is the only permanent (obligate) pathogen within the genus Bacillus. Its infection is a type of zoonosis, as it is transmitted from animals to humans. It was discovered by a German physician Robert Koch in 1876, and became the first bacterium to be experimentally shown as a pathogen. The discovery was also the first scientific evidence for the germ theory of diseases.

Tick-borne encephalitis vaccine is a vaccine used to prevent tick-borne encephalitis (TBE). The disease is most common in Central and Eastern Europe, and Northern Asia. More than 87% of people who receive the vaccine develop immunity. It is not useful following the bite of an infected tick. It is given by injection into a muscle.

Yellow fever vaccine is a vaccine that protects against yellow fever. Yellow fever is a viral infection that occurs in Africa and South America. Most people begin to develop immunity within ten days of vaccination and 99% are protected within one month, and this appears to be lifelong. The vaccine can be used to control outbreaks of disease. It is given either by injection into a muscle or just under the skin.

Anthrax vaccine adsorbed, sold under the brand name Biothrax among others, is a vaccine intended to provide acquired immunity against Bacillus anthracis.