ATC code J07Vaccines is a therapeutic subgroup of the Anatomical Therapeutic Chemical Classification System, a system of alphanumeric codes developed by the World Health Organization (WHO) for the classification of drugs and other medical products. Subgroup J07 is part of the anatomical group J Antiinfectives for systemic use.

The DPT vaccine or DTP vaccine is a class of combination vaccines against three infectious diseases in humans: diphtheria, pertussis, and tetanus. The vaccine components include diphtheria and tetanus toxoids and either killed whole cells of the bacterium that causes pertussis or pertussis antigens. The term toxoid refers to vaccines which use an inactivated toxin produced by the pathogen which they are targeted against to generate an immune response. In this way, the toxoid vaccine generates an immune response which is targeted against the toxin which is produced by the pathogen and causes disease, rather than a vaccine which is targeted against the pathogen itself. The whole cells or antigens will be depicted as either "DTwP" or "DTaP", where the lower-case "w" indicates whole-cell inactivated pertussis and the lower-case "a" stands for "acellular". In comparison to alternative vaccine types, such as live attenuated vaccines, the DTP vaccine does not contain the pathogen itself, but rather uses inactivated toxoid to generate an immune response; therefore, there is not a risk of use in populations that are immune compromised since there is not any known risk of causing the disease itself. As a result, the DTP vaccine is considered a safe vaccine to use in anyone and it generates a much more targeted immune response specific for the pathogen of interest.

Haemophilus influenzae is a Gram-negative, non-motile, coccobacillary, facultatively anaerobic, capnophilic pathogenic bacterium of the family Pasteurellaceae. The bacteria are mesophilic and grow best at temperatures between 35 and 37 °C.

A conjugate vaccine is a type of subunit vaccine which combines a weak antigen with a strong antigen as a carrier so that the immune system has a stronger response to the weak antigen.

Pneumococcal polysaccharide vaccine, sold under the brand name Pneumovax 23, is a pneumococcal vaccine that is used for the prevention of pneumococcal disease caused by the 23 serotypes of Streptococcus pneumoniae contained in the vaccine as capsular polysaccharides. It is given by intramuscular or subcutaneous injection.

The schedule for childhood immunizations in the United States is published by the Centers for Disease Control and Prevention (CDC). The vaccination schedule is broken down by age: birth to six years of age, seven to eighteen, and adults nineteen and older. Childhood immunizations are key in preventing diseases with epidemic potential.

Pneumococcal vaccines are vaccines against the bacterium Streptococcus pneumoniae. Their use can prevent some cases of pneumonia, meningitis, and sepsis. There are two types of pneumococcal vaccines: conjugate vaccines and polysaccharide vaccines. They are given by injection either into a muscle or just under the skin.

Hepatitis B vaccine is a vaccine that prevents hepatitis B. The first dose is recommended within 24 hours of birth with either two or three more doses given after that. This includes those with poor immune function such as from HIV/AIDS and those born premature. It is also recommended that health-care workers be vaccinated. In healthy people, routine immunization results in more than 95% of people being protected.
John Bennett Robbins was a senior investigator at the National Institutes of Health (NIH), best known for his contribution to the development of the vaccine against bacterial meningitis Hib)) with his colleague Rachel Schneerson. He conducted research on the Bethesda, Maryland campus of the NIH from 1970 until his retirement at the age of 80 in 2012. During his tenure, he worked in the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Food and Drug Administration’s biologics laboratories on location.
Pertussis vaccine is a vaccine that protects against whooping cough (pertussis). There are two main types: whole-cell vaccines and acellular vaccines. The whole-cell vaccine is about 78% effective while the acellular vaccine is 71–85% effective. The effectiveness of the vaccines appears to decrease by between 2 and 10% per year after vaccination with a more rapid decrease with the acellular vaccines. The vaccine is only available in combination with tetanus and diphtheria vaccines. Pertussis vaccine is estimated to have saved over 500,000 lives in 2002.
Meningococcal vaccine refers to any vaccine used to prevent infection by Neisseria meningitidis. Different versions are effective against some or all of the following types of meningococcus: A, B, C, W-135, and Y. The vaccines are between 85 and 100% effective for at least two years. They result in a decrease in meningitis and sepsis among populations where they are widely used. They are given either by injection into a muscle or just under the skin.
Haemophilus meningitis is a form of bacterial meningitis caused by the Haemophilus influenzae bacteria. It is usually associated with Haemophilus influenzae type b. Meningitis involves the inflammation of the protective membranes that cover the brain and spinal cord. Haemophilus meningitis is characterized by symptoms including fever, nausea, sensitivity to light, headaches, stiff neck, anorexia, and seizures. Haemophilus meningitis can be deadly, but antibiotics are effective in treating the infection, especially when cases are caught early enough that the inflammation has not done a great deal of damage. Before the introduction of the Hib vaccine in 1985, Haemophilus meningitis was the leading cause of bacterial meningitis in children under the age of five. However, since the creation of the Hib vaccine, only two in every 100,000 children contract this type of meningitis. Five to ten percent of cases can be fatal, although the average mortality rate in developing nations is seventeen percent, mostly due to lack of access to vaccination as well as lack of access to medical care needed to combat the meningitis.
A Vaccine Information Statement (VIS) is a document designed by the Centers for Disease Control and Prevention (CDC) to provide information to a patient receiving a vaccine in the United States. The National Childhood Vaccine Injury Act requires that medical professionals provide a VIS to patients before receiving certain vaccinations. The VIS includes information about the vaccine's benefits and risks, a description of the vaccine, indications and contraindications, instructions for patients experiencing an adverse reaction, and additional resources.
Tetanus vaccine, also known as tetanus toxoid (TT), is a toxoid vaccine used to prevent tetanus. During childhood, five doses are recommended, with a sixth given during adolescence.
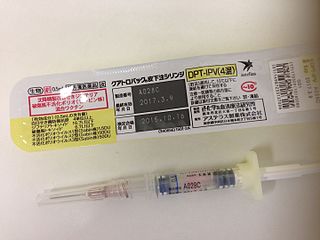
DTaP-IPV/Hib vaccine is a 5-in-1 combination vaccine that protects against diphtheria, tetanus, whooping cough, polio, and Haemophilus influenzae type B.
DTaP-IPV-HepB vaccine is a combination vaccine whose generic name is diphtheria and tetanus toxoids and acellular pertussis adsorbed, hepatitis B (recombinant) and inactivated polio vaccine or DTaP-IPV-Hep B. It protects against the infectious diseases diphtheria, tetanus, pertussis, poliomyelitis, and hepatitis B.
DPT-Hib vaccine is a combination vaccine whose generic name is diphtheria and tetanus toxoids and whole-cell pertussis vaccine adsorbed with Hib conjugate vaccine, sometimes abbreviated to DPT-Hib. It protects against the infectious diseases diphtheria, tetanus, pertussis, and Haemophilus influenzae type B.
DTaP-Hib vaccine is a combination vaccine whose generic name is diphtheria and tetanus toxoids and acellular pertussis adsorbed with Haemophilus B conjugate vaccine, sometimes abbreviated to DTaP-Hib. It protects against the infectious diseases diphtheria, tetanus, pertussis, and Haemophilus influenzae type B.

A hexavalent vaccine, or 6-in-1 vaccine, is a combination vaccine with six individual vaccines conjugated into one, intended to protect people from multiple diseases. The term usually refers to the children's vaccine that protects against diphtheria, tetanus, pertussis, poliomyelitis, haemophilus B, and hepatitis B, which is used in more than 90 countries around the world including in Europe, Canada, Australia, Jordan, and New Zealand.
Trudy Virginia Noller Murphy is an American pediatric infectious diseases physician, public health epidemiologist and vaccinologist. During the 1980s and 1990s, she conducted research at Southwestern Medical School in Dallas, Texas on three bacterial pathogens: Haemophilus influenzae type b (Hib), Streptococcus pneumoniae (pneumococcus), and methicillin-resistant Staphylococcus aureus (MRSA). Murphy's studies advanced understanding of how these organisms spread within communities, particularly among children attending day care centers. Her seminal work on Hib vaccines elucidated the effects of introduction of new Hib vaccines on both bacterial carriage and control of invasive Hib disease. Murphy subsequently joined the National Immunization Program at the Centers for Disease Control and Prevention (CDC). where she led multi-disciplinary teams in the Divisions of Epidemiology and Surveillance and The Viral Hepatitis Division. Among her most influential work at CDC was on Rotashield™, which was a newly licensed vaccine designed to prevent severe diarrheal disease caused by rotavirus. Murphy and her colleagues uncovered that the vaccine increased the risk of acute bowel obstruction (intussusception). This finding prompted suspension of the national recommendation to vaccinate children with Rotashield, and led the manufacturer to withdraw the vaccine from the market. For this work Murphy received the United States Department of Health and Human Services Secretary's Award for Distinguished Service in 2000, and the publication describing this work was recognized in 2002 by the Charles C. Shepard Science Award from the Centers for Disease Control and Prevention.