A urinary tract infection (UTI) is an infection that affects a part of the urinary tract. Lower urinary tract infections may involve the bladder (cystitis) or urethra (urethritis) while upper urinary tract infections affect the kidney (pyelonephritis). Symptoms from a lower urinary tract infection include suprapubic pain, painful urination (dysuria), frequency and urgency of urination despite having an empty bladder. Symptoms of a kidney infection, on the other hand, are more systemic and include fever or flank pain usually in addition to the symptoms of a lower UTI. Rarely, the urine may appear bloody. Symptoms may be vague or non-specific at the extremities of age.

Prostatitis is an umbrella term for a variety of medical conditions that incorporate bacterial and non-bacterial origin illnesses in the pelvic region. In contrast with the plain meaning of the word, the diagnosis may not always include inflammation. Prostatitis is classified into acute, chronic, asymptomatic inflammatory prostatitis, and chronic pelvic pain syndrome.

The prostate is both an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found in all male mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue, as well as connective tissue.
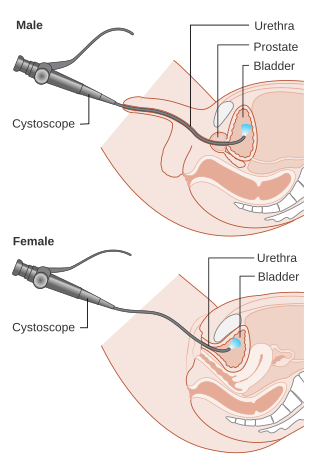
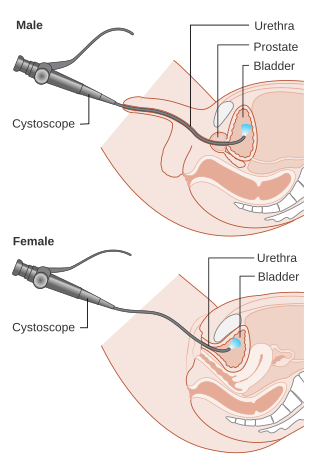
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes, most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.

In urinary catheterization, a latex, polyurethane, or silicone tube known as a urinary catheter is inserted into the bladder through the urethra to allow urine to drain from the bladder for collection. It may also be used to inject liquids used for treatment or diagnosis of bladder conditions. A clinician, often a nurse, usually performs the procedure, but self-catheterization is also possible. A catheter may be in place for long periods of time or removed after each use.

The seminal vesicles are a pair of convoluted tubular accessory glands that lie behind the urinary bladder of male mammals. They secrete fluid that partly composes the semen.
Bloodstream infections (BSIs) are infections of blood caused by blood-borne pathogens. The detection of microbes in the blood is always abnormal. A bloodstream infection is different from sepsis, which is characterized by severe inflammatory or immune responses of the host organism to pathogens.

Epididymitis is a medical condition characterized by inflammation of the epididymis, a curved structure at the back of the testicle. Onset of pain is typically over a day or two. The pain may improve with raising the testicle. Other symptoms may include swelling of the testicle, burning with urination, or frequent urination. Inflammation of the testicle is commonly also present.

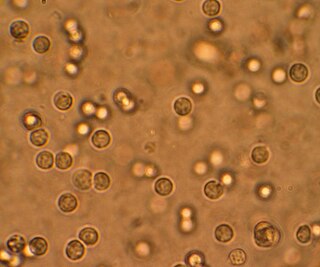
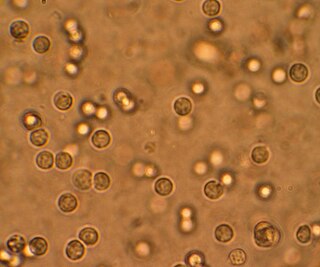
Hematuria or haematuria is defined as the presence of blood or red blood cells in the urine. "Gross hematuria" occurs when urine appears red, brown, or tea-colored due to the presence of blood. Hematuria may also be subtle and only detectable with a microscope or laboratory test. Blood that enters and mixes with the urine can come from any location within the urinary system, including the kidney, ureter, urinary bladder, urethra, and in men, the prostate. Common causes of hematuria include urinary tract infection (UTI), kidney stones, viral illness, trauma, bladder cancer, and exercise. These causes are grouped into glomerular and non-glomerular causes, depending on the involvement of the glomerulus of the kidney. But not all red urine is hematuria. Other substances such as certain medications and foods can cause urine to appear red. Menstruation in women may also cause the appearance of hematuria and may result in a positive urine dipstick test for hematuria. A urine dipstick test may also give an incorrect positive result for hematuria if there are other substances in the urine such as myoglobin, a protein excreted into urine during rhabdomyolysis. A positive urine dipstick test should be confirmed with microscopy, where hematuria is defined by three or more red blood cells per high power field. When hematuria is detected, a thorough history and physical examination with appropriate further evaluation can help determine the underlying cause.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.

Pyelonephritis is inflammation of the kidney, typically due to a bacterial infection. Symptoms most often include fever and flank tenderness. Other symptoms may include nausea, burning with urination, and frequent urination. Complications may include pus around the kidney, sepsis, or kidney failure.
Urethral syndrome is defined as symptoms suggestive of a lower urinary tract infection but in the absence of significant bacteriuria with a conventional pathogen. It is a diagnosis of exclusion in patients with dysuria and frequency without demonstrable infection. In women, vaginitis should also be ruled out.

Prostate biopsy is a procedure in which small hollow needle-core samples are removed from a man's prostate gland to be examined for the presence of prostate cancer. It is typically performed when the result from a PSA blood test is high. It may also be considered advisable after a digital rectal exam (DRE) finds possible abnormality. PSA screening is controversial as PSA may become elevated due to non-cancerous conditions such as benign prostatic hyperplasia (BPH), by infection, or by manipulation of the prostate during surgery or catheterization. Additionally many prostate cancers detected by screening develop so slowly that they would not cause problems during a man's lifetime, making the complications due to treatment unnecessary.
Prostatic congestion is a medical condition of the prostate gland that happens when the prostate becomes swollen by excess fluid and can be caused by prostatosis. The condition often results in a person with prostatic congestion feeling the urge to urinate frequently. Prostatic congestion has been associated with prostate disease, which can progress due to age. Oftentimes, the prostate will grow in size which can lead to further problems, such as prostatitis, enlarged prostate, or prostate cancer.

Chronic bacterial prostatitis is a bacterial infection of the prostate gland. It should be distinguished from other forms of prostatitis such as acute bacterial prostatitis and chronic pelvic pain syndrome (CPPS).

Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), previously known as chronic nonbacterial prostatitis, is long-term pelvic pain and lower urinary tract symptoms (LUTS) without evidence of a bacterial infection. It affects about 2–6% of men. Together with IC/BPS, it makes up urologic chronic pelvic pain syndrome (UCPPS).

Asymptomatic inflammatory prostatitis is a painless inflammation of the prostate gland where there is no evidence of infection. It should be distinguished from the other categories of prostatitis characterised by either pelvic pain or evidence of infection, such as chronic bacterial prostatitis, acute bacterial prostatitis and chronic pelvic pain syndrome (CPPS). It is a common finding in men with benign prostatic hyperplasia.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.

Emphysematous cystitis is a rare type of infection of the bladder wall by gas-forming bacteria or fungi. The most frequent offending organism is E. coli. Other gram negative bacteria, including Klebsiella and Proteus are also commonly isolated. Fungi, such as Candida, have also been reported as causative organisms. Citrobacter and Enterococci have also been found to cause emphysematous cystitis. Although it is a rare type of bladder infection, it is the most common type of all gas-forming bladder infections. The condition is characterized by the formation of air bubbles in and around the bladder wall. The gas found in the bladder consists of nitrogen, hydrogen, oxygen, and carbon dioxide. The disease most commonly affects elderly diabetic and immunocompromised patients. The first case was identified in a post-mortem examination in 1888.