A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, and enable mobility. Bones come in a variety of shapes and sizes and have complex internal and external structures. They are lightweight yet strong and hard and serve multiple functions.

A tendon or sinew is a tough band of dense fibrous connective tissue that connects muscle to bone. It sends the mechanical forces of muscle contraction to the skeletal system, while withstanding tension.
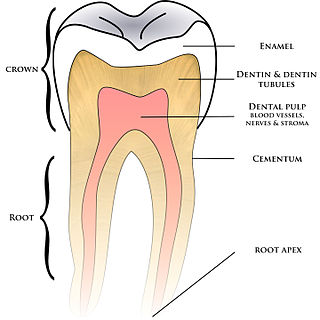
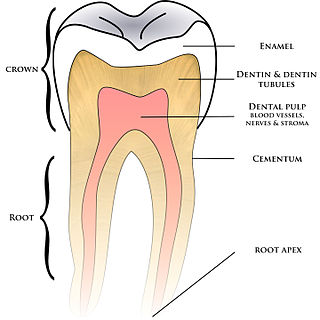
Cementum is a specialized calcified substance covering the root of a tooth. The cementum is the part of the periodontium that attaches the teeth to the alveolar bone by anchoring the periodontal ligament.
Osteoblasts are cells with a single nucleus that synthesize bone. However, in the process of bone formation, osteoblasts function in groups of connected cells. Individual cells cannot make bone. A group of organized osteoblasts together with the bone made by a unit of cells is usually called the osteon.

Dentin or dentine is a calcified tissue of the body and, along with enamel, cementum, and pulp, is one of the four major components of teeth. It is usually covered by enamel on the crown and cementum on the root and surrounds the entire pulp. By volume, 45% of dentin consists of the mineral hydroxyapatite, 33% is organic material, and 22% is water. Yellow in appearance, it greatly affects the color of a tooth due to the translucency of enamel. Dentin, which is less mineralized and less brittle than enamel, is necessary for the support of enamel. Dentin rates approximately 3 on the Mohs scale of mineral hardness. There are two main characteristics which distinguish dentin from enamel: firstly, dentin forms throughout life; secondly, dentin is sensitive and can become hypersensitive to changes in temperature due to the sensory function of odontoblasts, especially when enamel recedes and dentin channels become exposed.

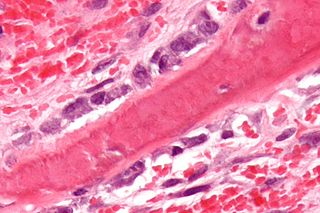
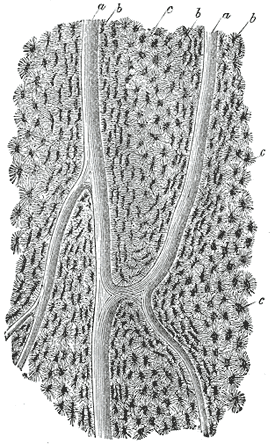
An osteocyte, an oblate shaped type of bone cell with dendritic processes, is the most commonly found cell in mature bone. It can live as long as the organism itself. The adult human body has about 42 billion of them. Osteocytes do not divide and have an average half life of 25 years. They are derived from osteoprogenitor cells, some of which differentiate into active osteoblasts. Osteoblasts/osteocytes develop in mesenchyme.

The pulp is the connective tissue, nerves, blood vessels, and odontoblasts that comprise the innermost layer of a tooth. The pulp's activity and signalling processes regulate its behaviour.

Intramembranous ossification is one of the two essential processes during fetal development of the gnathostome skeletal system by which rudimentary bone tissue is created. Intramembranous ossification is also an essential process during the natural healing of bone fractures and the rudimentary formation of bones of the head.

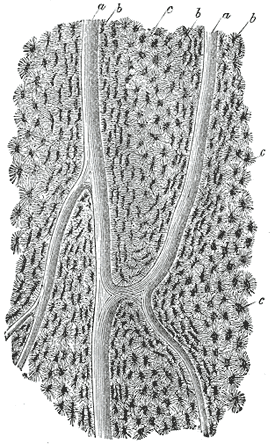
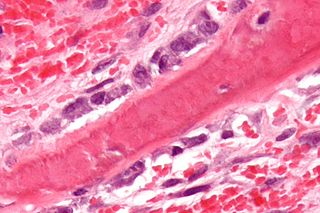
In osteology, the osteon or haversian system is the fundamental functional unit of much compact bone. Osteons are roughly cylindrical structures that are typically between 0.25 mm and 0.35 mm in diameter. Their length is often hard to define, but estimates vary from several millimeters to around 1 centimeter. They are present in many bones of most mammals and some bird, reptile, and amphibian species.

Haversian canals are a series of microscopic tubes in the outermost region of bone called cortical bone. They allow blood vessels and nerves to travel through them to supply the osteocytes.

In vertebrates, an odontoblast is a cell of neural crest origin that is part of the outer surface of the dental pulp, and whose biological function is dentinogenesis, which is the formation of dentin, the substance beneath the tooth enamel on the crown and the cementum on the root.
Pulpitis is inflammation of dental pulp tissue. The pulp contains the blood vessels, the nerves, and connective tissue inside a tooth and provides the tooth's blood and nutrients. Pulpitis is mainly caused by bacterial infection which itself is a secondary development of caries. It manifests itself in the form of a toothache.

Thrinaxodon is an extinct genus of cynodonts, including the species T. liorhinus which lived in what are now South Africa and Antarctica during the Early Triassic. Thrinaxodon lived just after the Permian–Triassic mass extinction event, its survival during the extinction may have been due to its burrowing habits.
A cementoblast is a biological cell that forms from the follicular cells around the root of a tooth, and whose biological function is cementogenesis, which is the formation of cementum. The mechanism of differentiation of the cementoblasts is controversial but circumstantial evidence suggests that an epithelium or epithelial component may cause dental sac cells to differentiate into cementoblasts, characterised by an increase in length. Other theories involve Hertwig epithelial root sheath (HERS) being involved.

Bone resorption is resorption of bone tissue, that is, the process by which osteoclasts break down the tissue in bones and release the minerals, resulting in a transfer of calcium from bone tissue to the blood.

Dentinogenesis imperfecta (DI) is a genetic disorder of tooth development. It is inherited in an autosomal dominant pattern, as a result of mutations on chromosome 4q21, in the dentine sialophosphoprotein gene (DSPP). It is one of the most frequently occurring autosomal dominant features in humans. Dentinogenesis imperfecta affects an estimated 1 in 6,000-8,000 people.
Dentin hypersensitivity is dental pain which is sharp in character and of short duration, arising from exposed dentin surfaces in response to stimuli, typically thermal, evaporative, tactile, osmotic, chemical or electrical; and which cannot be ascribed to any other dental disease.
In histology, a lacuna is a small space, containing an osteocyte in bone, or chondrocyte in cartilage.
In dentistry, the hydrodynamic or fluid movement theory is one of three main theories developed to explain dentine hypersensitivity, which is a sharp, transient pain arising from stimuli exposure. It states that different types of stimuli act on exposed dentine, causing increased fluid flow through the dentinal tubules. In response to this movement, mechanoreceptors on the pulp nerves trigger the acute, temporary pain of dentine hypersensitivity.
In dentistry, the smear layer is a layer found on root canal walls after root canal instrumentation. It consists of microcrystalline and organic particle debris. It was first described in 1975 and research has been performed since then to evaluate its importance in bacteria penetration into the dentinal tubules and its effects on endodontic treatment. More broadly, it is the organic layer found over all hard tooth surfaces.