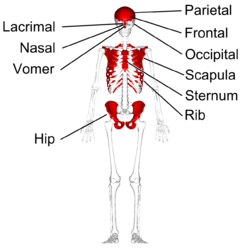
A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, and enable mobility. Bones come in a variety of shapes and sizes and have complex internal and external structures. They are lightweight yet strong and hard and serve multiple functions.

A skeleton is the structural frame that supports the body of most animals. There are several types of skeletons, including the exoskeleton, which is a rigid outer shell that holds up an organism's shape; the endoskeleton, a rigid internal frame to which the organs and soft tissues attach; and the hydroskeleton, a flexible internal structure supported by the hydrostatic pressure of body fluids.

Bone healing, or fracture healing, is a proliferative physiological process in which the body facilitates the repair of a bone fracture.

Parathyroid hormone (PTH), also called parathormone or parathyrin, is a peptide hormone secreted by the parathyroid glands that regulates the serum calcium concentration through its effects on bone, kidney, and intestine.
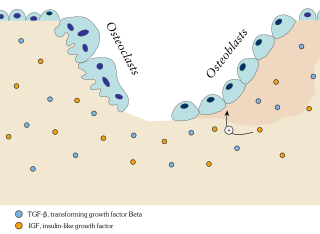
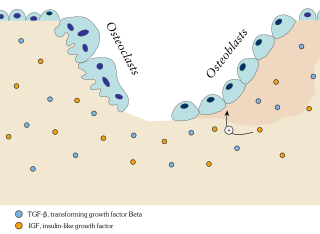
Osteoblasts are cells with a single nucleus that synthesize bone. However, in the process of bone formation, osteoblasts function in groups of connected cells. Individual cells cannot make bone. A group of organized osteoblasts together with the bone made by a unit of cells is usually called the osteon.

An osteoclast is a type of bone cell that breaks down bone tissue. This function is critical in the maintenance, repair, and remodeling of bones of the vertebral skeleton. The osteoclast disassembles and digests the composite of hydrated protein and mineral at a molecular level by secreting acid and a collagenase, a process known as bone resorption. This process also helps regulate the level of blood calcium.

The periosteum is a membrane that covers the outer surface of all bones, except at the articular surfaces of long bones. Endosteum lines the inner surface of the medullary cavity of all long bones.

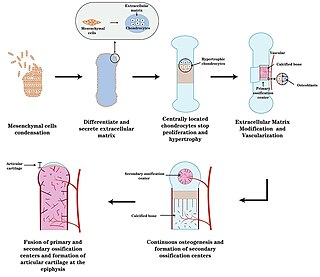
The long bones are those that are longer than they are wide. They are one of five types of bones: long, short, flat, irregular and sesamoid. Long bones, especially the femur and tibia, are subjected to most of the load during daily activities and they are crucial for skeletal mobility. They grow primarily by elongation of the diaphysis, with an epiphysis at each end of the growing bone. The ends of epiphyses are covered with hyaline cartilage. The longitudinal growth of long bones is a result of endochondral ossification at the epiphyseal plate. Bone growth in length is stimulated by the production of growth hormone (GH), a secretion of the anterior lobe of the pituitary gland.

An osteocyte, an oblate shaped type of bone cell with dendritic processes, is the most commonly found cell in mature bone. It can live as long as the organism itself. The adult human body has about 42 billion of them. Osteocytes do not divide and have an average half life of 25 years. They are derived from osteoprogenitor cells, some of which differentiate into active osteoblasts. Osteoblasts/osteocytes develop in mesenchyme.
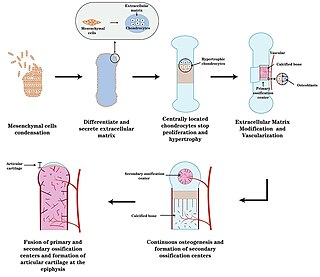
Endochondral ossification is one of the two essential pathways by which bone tissue is produced during fetal development of the mammalian skeletal system, the other pathway being intramembranous ossification. Both endochondral and intramembranous processes initiate from a precursor mesenchymal tissue, but their transformations into bone are different. In intramembranous ossification, mesenchymal tissue is directly converted into bone. On the other hand, endochondral ossification starts with mesenchymal tissue turning into an intermediate cartilage stage, which is eventually substituted by bone.

Intramembranous ossification is one of the two essential processes during fetal development of the gnathostome skeletal system by which rudimentary bone tissue is created. Intramembranous ossification is also an essential process during the natural healing of bone fractures and the rudimentary formation of bones of the head.

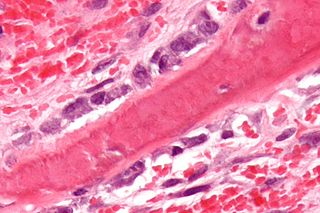
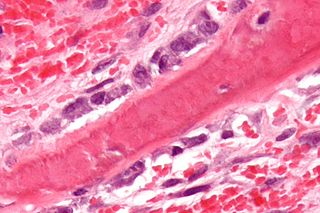
In osteology, the osteon or haversian system is the fundamental functional unit of much compact bone. Osteons are roughly cylindrical structures that are typically between 0.25 mm and 0.35 mm in diameter. Their length is often hard to define, but estimates vary from several millimeters to around 1 centimeter. They are present in many bones of most mammals and some bird, reptile, and amphibian species.
Ossification in bone remodeling is the process of laying down new bone material by cells named osteoblasts. It is synonymous with bone tissue formation. There are two processes resulting in the formation of normal, healthy bone tissue: Intramembranous ossification is the direct laying down of bone into the primitive connective tissue (mesenchyme), while endochondral ossification involves cartilage as a precursor.

The dental follicle, also known as dental sac, is made up of mesenchymal cells and fibres surrounding the enamel organ and dental papilla of a developing tooth. It is a vascular fibrous sac containing the developing tooth and its odontogenic organ. The dental follicle (DF) differentiates into the periodontal ligament. In addition, it may be the precursor of other cells of the periodontium, including osteoblasts, cementoblasts and fibroblasts. They develop into the alveolar bone, the cementum with Sharpey's fibers and the periodontal ligament fibers respectively. Similar to dental papilla, the dental follicle provides nutrition to the enamel organ and dental papilla and also have an extremely rich blood supply.

Bone grafting is a surgical procedure that replaces missing bone in order to repair bone fractures that are extremely complex, pose a significant health risk to the patient, or fail to heal properly. Some small or acute fractures can be cured without bone grafting, but the risk is greater for large fractures like compound fractures.

The alveolar process is the portion of bone containing the tooth sockets on the jaw bones. The alveolar process is covered by gums within the mouth, terminating roughly along the line of the mandibular canal. Partially comprising compact bone, it is penetrated by many small openings for blood vessels and connective fibres.

Bone resorption is resorption of bone tissue, that is, the process by which osteoclasts break down the tissue in bones and release the minerals, resulting in a transfer of calcium from bone tissue to the blood.

The endosteum is a thin vascular membrane of connective tissue that lines the inner surface of the bony tissue that forms the medullary cavity of long bones.
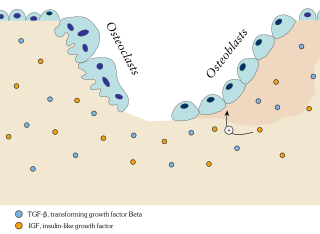
In osteology, bone remodeling or bone metabolism is a lifelong process where mature bone tissue is removed from the skeleton and new bone tissue is formed. Recent research has identified a specialised subset of blood vessels, termed Type R endothelial cells, in the bone microenvironment. These blood vessels play a crucial role in adult bone remodelling by mediating interactions between bone-resorbing osteoclasts and bone-forming osteoblasts. Type R blood vessels are characterised by their association with post-arterial capillaries and exhibit unique remodelling properties crucial for bone homeostasis. These processes also control the reshaping or replacement of bone following injuries like fractures but also micro-damage, which occurs during normal activity. Remodeling responds also to functional demands of the mechanical loading.
Hard tissue, refers to "normal" calcified tissue, is the tissue which is mineralized and has a firm intercellular matrix. The hard tissues of humans are bone, tooth enamel, dentin, and cementum. The term is in contrast to soft tissue.