An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.

A cerebral arteriovenous malformation is an abnormal connection between the arteries and veins in the brain—specifically, an arteriovenous malformation in the cerebrum.

Veins are blood vessels in the circulatory system of humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation, arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.

The dura mater, is the outermost of the three meningeal membranes. The dura mater has two layers, an outer periosteal layer closely adhered to the neurocranium, and an inner meningeal layer known as the dural border cell layer. The two dural layers are for the most part fused together forming a thick fibrous tissue membrane that covers the brain and the vertebrae of the spinal column. But the layers are separated at the dural venous sinuses to allow blood to drain from the brain. The dura covers the arachnoid mater and the pia mater the other two meninges in protecting the central nervous system.
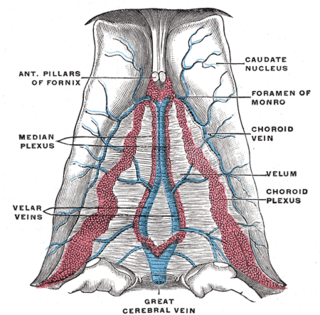
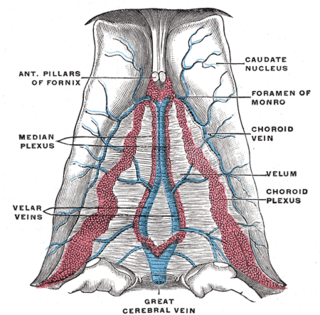
The great cerebral vein is one of the large blood vessels in the skull draining the cerebrum of the brain. It is also known as the vein of Galen, named for its discoverer, the Greek physician Galen.

Cerebral circulation is the movement of blood through a network of cerebral arteries and veins supplying the brain. The rate of cerebral blood flow in an adult human is typically 750 milliliters per minute, or about 15% of cardiac output. Arteries deliver oxygenated blood, glucose and other nutrients to the brain. Veins carry "used or spent" blood back to the heart, to remove carbon dioxide, lactic acid, and other metabolic products. The neurovascular unit regulates cerebral blood flow so that activated neurons can be supplied with energy in the right amount and at the right time. Because the brain would quickly suffer damage from any stoppage in blood supply, the cerebral circulatory system has safeguards including autoregulation of the blood vessels. The failure of these safeguards may result in a stroke. The volume of blood in circulation is called the cerebral blood flow. Sudden intense accelerations change the gravitational forces perceived by bodies and can severely impair cerebral circulation and normal functions to the point of becoming serious life-threatening conditions.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.

An arteriovenous fistula is an abnormal connection or passageway between an artery and a vein. It may be congenital, surgically created for hemodialysis treatments, or acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm.
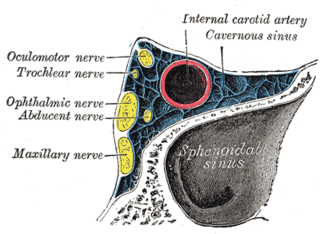
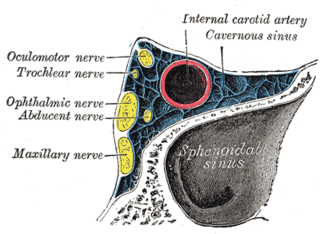
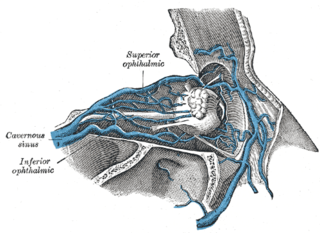
A carotid-cavernous fistula results from an abnormal communication between the arterial and venous systems within the cavernous sinus in the skull. It is a type of arteriovenous fistula. As arterial blood under high pressure enters the cavernous sinus, the normal venous return to the cavernous sinus is impeded and this causes engorgement of the draining veins, manifesting most dramatically as a sudden engorgement and redness of the eye of the same side.
The cavernous sinus within the human head is one of the dural venous sinuses creating a cavity called the lateral sellar compartment bordered by the temporal bone of the skull and the sphenoid bone, lateral to the sella turcica.

The dural venous sinuses are venous sinuses (channels) found between the periosteal and meningeal layers of dura mater in the brain. They receive blood from the cerebral veins, and cerebrospinal fluid (CSF) from the subarachnoid space via arachnoid granulations. They mainly empty into the internal jugular vein. Cranial venous sinuses communicate with veins outside the skull through emissary veins. These communications help to keep the pressure of blood in the sinuses constant.
The confluence of sinuses, torcular Herophili, or torcula is the connecting point of the superior sagittal sinus, straight sinus, and occipital sinus. It is below the internal occipital protuberance of the skull. It drains venous blood from the brain into the transverse sinuses. It may be affected by arteriovenous fistulas, a thrombus, major trauma, or surgical damage, and may be imaged with many radiology techniques.
The superior petrosal sinus is one of the dural venous sinuses located beneath the brain. It receives blood from the cavernous sinus and passes backward and laterally to drain into the transverse sinus. The sinus receives superior petrosal veins, some cerebellar veins, some inferior cerebral veins, and veins from the tympanic cavity. They may be affected by arteriovenous malformation or arteriovenous fistula, usually treated with surgery.

The cerebellar veins are veins which drain the cerebellum. They consist of the superior cerebellar veins and the inferior cerebellar veins. The superior cerebellar veins drain to the straight sinus and the internal cerebral veins. The inferior cerebellar veins drain to the transverse sinus, the superior petrosal sinus, and the occipital sinus.
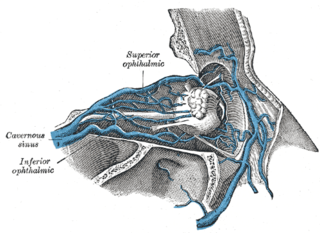
The nasofrontal vein is a vein in the orbit around the eye. It drains into the superior ophthalmic vein. It can be used for endovascular access to the cavernous sinus.
A vascular malformation is a type of vascular anomaly. They may cause aesthetic problems as they have a growth cycle, and can continue to grow throughout life.
Vascular myelopathy refers to an abnormality of the spinal cord in regard to its blood supply. The blood supply is complicated and supplied by two major vessel groups: the posterior spinal arteries and the anterior spinal arteries—of which the Artery of Adamkiewicz is the largest. Both the posterior and anterior spinal arteries run the entire length of the spinal cord and receive anastomotic (conjoined) vessels in many places. The anterior spinal artery has a less efficient supply of blood and is therefore more susceptible to vascular disease. Whilst atherosclerosis of spinal arteries is rare, necrosis in the anterior artery can be caused by disease in vessels originating from the segmental arteries such as atheroma or aortic dissection.

Vein of Galen aneurysmal malformations(VGAMs) and Vein of Galen aneurysmal dilations (VGADs) are the most frequent arteriovenous malformations in infants and fetuses. A VGAM consists of a tangled mass of dilated vessels supplied by an enlarged artery. The malformation increases greatly in size with age, although the mechanism of the increase is unknown. Dilation of the great cerebral vein of Galen is a secondary result of the force of arterial blood either directly from an artery via an arteriovenous fistula or by way of a tributary vein that receives the blood directly from an artery. There is usually a venous anomaly downstream from the draining vein that, together with the high blood flow into the great cerebral vein of Galen causes its dilation. The right sided cardiac chambers and pulmonary arteries also develop mild to severe dilation.
Alexander Coon is an American neurosurgeon who is the director of endovascular and cerebrovascular neurosurgery at the Carondelet Neurological Institute of St. Joseph's and St. Mary's Hospitals in Tucson, Arizona. He was previously the director of endovascular neurosurgery at the Johns Hopkins Hospital and an assistant professor of neurosurgery, neurology, and radiology at the Johns Hopkins Hospital. He is known for his work in cerebrovascular and endovascular neurosurgery and his research in neuroendovascular devices and clinical outcomes in the treatment of cerebral aneurysms, subarachnoid hemorrhage, and AVMs.