Related Research Articles
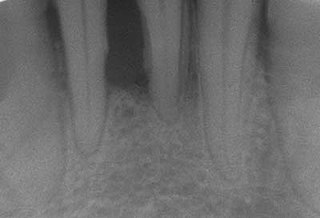
Periodontal disease, also known as gum disease, is a set of inflammatory conditions affecting the tissues surrounding the teeth. In its early stage, called gingivitis, the gums become swollen and red and may bleed. It is considered the main cause of tooth loss for adults worldwide. In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or fall out. Halitosis may also occur.

Toothaches, also known as dental pain or tooth pain, is pain in the teeth or their supporting structures, caused by dental diseases or pain referred to the teeth by non-dental diseases. When severe it may impact sleep, eating, and other daily activities.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A periodontist is a dentist that specializes in the prevention, diagnosis and treatment of periodontal disease and in the placement of dental implants.
Dental plaque is a biofilm of microorganisms that grows on surfaces within the mouth. It is a sticky colorless deposit at first, but when it forms tartar, it is often brown or pale yellow. It is commonly found between the teeth, on the front of teeth, behind teeth, on chewing surfaces, along the gumline (supragingival), or below the gumline cervical margins (subgingival). Dental plaque is also known as microbial plaque, oral biofilm, dental biofilm, dental plaque biofilm or bacterial plaque biofilm. Bacterial plaque is one of the major causes for dental decay and gum disease.

In dental anatomy, the gingival sulcus is an area of potential space between a tooth and the surrounding gingival tissue and is lined by sulcular epithelium. The depth of the sulcus is bounded by two entities: apically by the gingival fibers of the connective tissue attachment and coronally by the free gingival margin. A healthy sulcular depth is three millimeters or less, which is readily self-cleansable with a properly used toothbrush or the supplemental use of other oral hygiene aids.

In dental anatomy, the gingival and periodontal pockets are dental terms indicating the presence of an abnormal depth of the gingival sulcus near the point at which the gingival (gum) tissue contacts the tooth.

Scaling and root planing, also known as conventional periodontal therapy, non-surgical periodontal therapy or deep cleaning, is a procedure involving removal of dental plaque and calculus and then smoothing, or planing, of the (exposed) surfaces of the roots, removing cementum or dentine that is impregnated with calculus, toxins, or microorganisms, the agents that cause inflammation. It is a part of non-surgical periodontal therapy. This helps to establish a periodontium that is in remission of periodontal disease. Periodontal scalers and periodontal curettes are some of the tools involved.

Oral hygiene is the practice of keeping one's oral cavity clean and free of disease and other problems by regular brushing of the teeth and adopting good hygiene habits. It is important that oral hygiene be carried out on a regular basis to enable prevention of dental disease and bad breath. The most common types of dental disease are tooth decay and gum diseases, including gingivitis, and periodontitis.
Laser-assisted new attachment procedure (LANAP) is a surgical therapy for the treatment of periodontitis, intended to work through regeneration rather than resection. This therapy and the laser used to perform it have been in use since 1994. It was developed by Robert H. Gregg II and Delwin McCarthy.

Gingivitis is a non-destructive disease that causes inflammation of the gums; ulitis is an alternative term. The most common form of gingivitis, and the most common form of periodontal disease overall, is in response to bacterial biofilms that are attached to tooth surfaces, termed plaque-induced gingivitis. Most forms of gingivitis are plaque-induced.

In dentistry, debridement refers to the removal by dental cleaning of accumulations of plaque and calculus (tartar) in order to maintain dental health. Debridement may be performed using ultrasonic instruments, which fracture the calculus, thereby facilitating its removal, as well as hand tools, including periodontal scaler and curettes, or through the use of chemicals such as hydrogen peroxide.
Epidemiology of periodontal disease is the study of patterns, causes, and effects of periodontal diseases. Periodontal disease is a disease affecting the tissue surrounding the teeth. This causes the gums and the teeth to separate making spaces that become infected. The immune system tries to fight the toxins breaking down the bone and tissue connecting to the teeth to the gums. The teeth will have to be removed. This is an advance stage of gum disease that has multiple definitions. Adult periodontitis affects less than 10 to 15% of the population in industrialized countries, mainly adults around the ages of 50 to 60. The disease is now declining world-wide.

A periodontal abscess, is a localized collection of pus within the tissues of the periodontium. It is a type of dental abscess. A periodontal abscess occurs alongside a tooth, and is different from the more common periapical abscess, which represents the spread of infection from a dead tooth. To reflect this, sometimes the term "lateral (periodontal) abscess" is used. In contrast to a periapical abscess, periodontal abscesses are usually associated with a vital (living) tooth. Abscesses of the periodontium are acute bacterial infections classified primarily by location.
Chronic periodontitis is one of the seven categories of periodontitis as defined by the American Academy of Periodontology 1999 classification system. Chronic periodontitis is a common disease of the oral cavity consisting of chronic inflammation of the periodontal tissues that is caused by the accumulation of profuse amounts of dental plaque. Periodontitis initially begins as gingivitis and can progress onto chronic and subsequent aggressive periodontitis according to the 1999 classification.
Aggressive periodontitis describes a type of periodontal disease and includes two of the seven classifications of periodontitis as defined by the 1999 classification system:
- Localized aggressive periodontitis (LAP)
- Generalized aggressive periodontitis (GAP)
Host modulatory therapy is an emerging treatment concept in the management of periodontitis that aims to reduce tissue destruction and stabilise or even regenerate the periodontium by modifying the host response. Historically treatment of periodontitis has been focused on reducing the bacterial challenge. However the outcomes of the conventional treatment procedures like scaling and root planning (SRP) are not always stable or predictable. Periodontal disease is seen as a balance between (1) a persisting bacterial challenge and the proinflammatory destructive events in the tissue and (2) resolution of inflammation and downregulation of destructive processes. The goal is to maximize treatment response by reducing inflammation and inhibiting destructive processes in the tissues which will result in enhanced periodontal stability after conventional periodontal treatments like SRP.
Impacted wisdom teeth is a condition where the third molars are prevented from erupting into the mouth. This can be caused by a physical barrier, such as other teeth, or when the tooth is angled away from a vertical position. Completely unerupted wisdom teeth usually result in no symptoms, although they can sometimes develop cysts or neoplasms. Partially erupted wisdom teeth or wisdom teeth that are not erupted but are exposed to oral bacteria through deep periodontal pocket, can develop cavities or pericoronitis. Removal of impacted wisdom teeth is advised for the future prevention of or in the current presence of certain pathologies, such as caries, periodontal disease or cysts. Prophylactic (preventative) extraction of wisdom teeth is preferred to be done at a younger age to take advantage of incomplete root development, which is associated with an easier surgical procedure and less probability of complications.
There are many circumstances during dental treatment where antibiotics are prescribed by dentists to prevent further infection. The most common antibiotic prescribed by dental practitioners is penicillin in the form of amoxicillin, however many patients are hypersensitive to this particular antibiotic. Therefore, in the cases of allergies, erythromycin is used instead.

Jørgen Slots is a Danish-born periodontist notable for his contributions to the field of periodontology. He is currently professor of periodontology and microbiology at the Herman Ostrow School of Dentistry of USC, and served as chairman of periodontology from 1991 to 2001.
References
- ↑ Jervøe-Storm, Pia-Merete; Eberhard, Jörg; Needleman, Ian; Worthington, Helen V.; Jepsen, Søren (2022-06-28). "Full-mouth treatment modalities (within 24 hours) for periodontitis in adults". The Cochrane Database of Systematic Reviews. 2022 (6): CD004622. doi:10.1002/14651858.CD004622.pub4. ISSN 1469-493X. PMC 9239328 . PMID 35763286.