Related Research Articles

Miscarriage, also known in medical terms as a spontaneous abortion, is the death and expulsion of an embryo or fetus before it is able to survive independently. The term miscarriage is sometimes used to refer to all forms of pregnancy loss and pregnancy with abortive outcome before 20 weeks of gestation.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

Human chorionic gonadotropin (hCG) is a hormone for the maternal recognition of pregnancy produced by trophoblast cells that are surrounding a growing embryo, which eventually forms the placenta after implantation. The presence of hCG is detected in some pregnancy tests. Some cancerous tumors produce this hormone; therefore, elevated levels measured when the patient is not pregnant may lead to a cancer diagnosis and, if high enough, paraneoplastic syndromes, however, it is not known whether this production is a contributing cause, or an effect of carcinogenesis. The pituitary analog of hCG, known as luteinizing hormone (LH), is produced in the pituitary gland of males and females of all ages.

A pregnancy test is used to determine whether a female is pregnant or not. The two primary methods are testing for the female pregnancy hormone in blood or urine using a pregnancy test kit, and scanning with ultrasonography. Testing blood for hCG results in the earliest detection of pregnancy. Almost all pregnant women will have a positive urine pregnancy test one week after the first day of a missed menstrual period.

The trophoblast is the outer layer of cells of the blastocyst. Trophoblasts are present four days after fertilization in humans. They provide nutrients to the embryo and develop into a large part of the placenta. They form during the first stage of pregnancy and are the first cells to differentiate from the fertilized egg to become extraembryonic structures that do not directly contribute to the embryo. After blastulation, the trophoblast is contiguous with the ectoderm of the embryo and is referred to as the trophectoderm. After the first differentiation, the cells in the human embryo lose their totipotency because they can no longer form a trophoblast. They become pluripotent stem cells.

A molar pregnancy, also known as a hydatidiform mole, is an abnormal form of pregnancy in which a non-viable fertilized egg implants in the uterus. It falls under the category of gestational trophoblastic diseases and was previously known as a hydatidiform mole. During a molar pregnancy, the uterus contains a growing mass characterized by swollen chorionic villi, resembling clusters of grapes. The occurrence of a molar pregnancy can be attributed to the fertilized egg lacking an original maternal nucleus. As a result, the products of conception may or may not contain fetal tissue. These molar pregnancies are categorized into two types: partial moles and complete moles, where the term 'mole' simply denotes a clump of growing tissue or a ‘growth'.

Choriocarcinoma is a malignant, trophoblastic cancer, usually of the placenta. It is characterized by early hematogenous spread to the lungs. It belongs to the malignant end of the spectrum in gestational trophoblastic disease (GTD). It is also classified as a germ cell tumor and may arise in the testis or ovary.
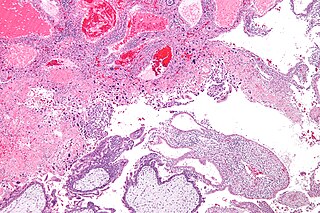
Gestational trophoblastic disease (GTD) is a term used for a group of pregnancy-related tumours. These tumours are rare, and they appear when cells in the womb start to proliferate uncontrollably. The cells that form gestational trophoblastic tumours are called trophoblasts and come from tissue that grows to form the placenta during pregnancy.

A seminoma is a germ cell tumor of the testicle or, more rarely, the mediastinum or other extra-gonadal locations. It is a malignant neoplasm and is one of the most treatable and curable cancers, with a survival rate above 95% if discovered in early stages.

Dactinomycin, also known as actinomycin D, is a chemotherapy medication used to treat a number of types of cancer. This includes Wilms tumor, rhabdomyosarcoma, Ewing's sarcoma, trophoblastic neoplasm, testicular cancer, and certain types of ovarian cancer. It is given by injection into a vein.
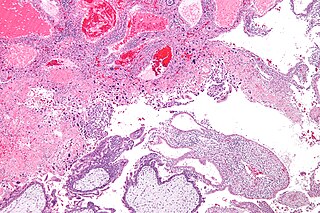
Gestational trophoblastic neoplasia (GTN) is group of rare diseases related to pregnancy and included in gestational trophoblastic disease (GTD) in which abnormal trophoblast cells grow in the uterus. GTN can be classified into benign and malignant lesions. Benign lesions include placental site nodule and hydatidiform moles while malignant lesions have four subtypes including invasive mole, gestational choriocarcinoma, placental site trophoblastic tumor (PSTT) and epithelioid trophoblastic tumor (ETT). The choriocarcinoma has 2 significant subtypes including gestational and non-gestational and they are differentiated by their different biological feature and prognosis. Signs and symptoms of GTN will appear vary from person to person and depending upon the type of the disease. They may include uterine bleeding not related to menstruation, pain or pressure in pelvis, large uterus and high blood pressure during pregnancy. The cause of this disease is unknown but the identification of the tumor based on total beta-human chorionic gonadotropin (β-hCG) in the serum.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

"Cytotrophoblast" is the name given to both the inner layer of the trophoblast or the cells that live there. It is interior to the syncytiotrophoblast and external to the wall of the blastocyst in a developing embryo.

A placental disease is any disease, disorder, or pathology of the placenta.

An interstitial pregnancy is a uterine but ectopic pregnancy; the pregnancy is located outside the uterine cavity in that part of the fallopian tube that penetrates the muscular layer of the uterus. The term cornual pregnancy is sometimes used as a synonym, but remains ambiguous as it is also applied to indicate the presence of a pregnancy located within the cavity in one of the two upper "horns" of a bicornuate uterus. Interstitial pregnancies have a higher mortality than ectopics in general.

Placental site trophoblastic tumor is a form of gestational trophoblastic disease, which is thought to arise from intermediate trophoblast.
Theca lutein cyst is a type of bilateral functional ovarian cyst filled with clear, straw-colored fluid. These cysts result from exaggerated physiological stimulation due to elevated levels of beta-human chorionic gonadotropin (beta-hCG) or hypersensitivity to beta-hCG. On ultrasound and MRI, theca lutein cysts appear in multiples on ovaries that are enlarged.

Min Chiu Li was a Chinese-American oncologist and cancer researcher. Li was the first scientist to use chemotherapy to cure widely metastatic, malignant cancer.
Early pregnancy bleeding refers to vaginal bleeding before 14 weeks of gestational age. If the bleeding is significant, hemorrhagic shock may occur. Concern for shock is increased in those who have loss of consciousness, chest pain, shortness of breath, or shoulder pain.
Epithelioid trophoblastic tumor (ETT) is a gestational trophoblastic disease with about 110 case reports in the literature. It is a trophoblastic tumor of neoplastic chorionic type associated with the intermediate trophoblast.
References
- ↑ Sharami SR, Saffarieh E (March 2020). "A review on management of gestational trophoblastic neoplasia". Journal of Family Medicine and Primary Care. 9 (3): 1287–1295. doi: 10.4103/jfmpc.jfmpc_876_19 . PMC 7266251 . PMID 32509606.
- 1 2 3 Braga A, Mora P, de Melo AC, Nogueira-Rodrigues A, Amim-Junior J, Rezende-Filho J, Seckl MJ (February 2019). "Challenges in the diagnosis and treatment of gestational trophoblastic neoplasia worldwide". World Journal of Clinical Oncology. 10 (2): 28–37. doi: 10.5306/wjco.v10.i2.28 . PMC 6390119 . PMID 30815369.
- 1 2 3 4 Hui P (January 2019). "Gestational Trophoblastic Tumors: A Timely Review of Diagnostic Pathology". Archives of Pathology & Laboratory Medicine. 143 (1): 65–74. doi: 10.5858/arpa.2018-0234-RA . PMID 30407075. S2CID 53213943.
- 1 2 3 4 5 Ngan HY, Seckl MJ, Berkowitz RS, Xiang Y, Golfier F, Sekharan PK, et al. (October 2018). "Update on the diagnosis and management of gestational trophoblastic disease". International Journal of Gynaecology and Obstetrics. 143 (Suppl 2): 79–85. doi: 10.1002/ijgo.12615 . PMID 30306586. S2CID 52958887.
- ↑ Shaaban AM, Rezvani M, Haroun RR, Kennedy AM, Elsayes KM, Olpin JD, et al. (2017). "Gestational Trophoblastic Disease: Clinical and Imaging Features". Radiographics. 37 (2): 681–700. doi:10.1148/rg.2017160140. PMID 28287945.
- 1 2 3 4 5 6 7 Tsakiridis I, Giouleka S, Kalogiannidis I, Mamopoulos A, Athanasiadis A, Dagklis T (December 2020). "Diagnosis and Management of Gestational Trophoblastic Disease: A Comparative Review of National and International Guidelines". Obstetrical & Gynecological Survey. 75 (12): 747–756. doi:10.1097/OGX.0000000000000848. PMID 33369685. S2CID 229380333.
- 1 2 3 4 5 Lok C, Frijstein M, van Trommel N (July 2021). "Clinical presentation and diagnosis of Gestational Trophoblastic Disease". Best Practice & Research. Clinical Obstetrics & Gynaecology. 74: 42–52. doi:10.1016/j.bpobgyn.2020.12.001. PMID 33422446. S2CID 231577251.
- ↑ Ning F, Hou H, Morse AN, Lash GE (2019). "Understanding and management of gestational trophoblastic disease". F1000Research. 8: F1000 Faculty Rev–428. doi: 10.12688/f1000research.14953.1 . PMC 6464061 . PMID 31001418.
- 1 2 3 4 5 Lurain JR (December 2010). "Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole". American Journal of Obstetrics and Gynecology. 203 (6): 531–539. doi:10.1016/j.ajog.2010.06.073. PMID 20728069.
- 1 2 3 4 5 6 Altieri A, Franceschi S, Ferlay J, Smith J, La Vecchia C (November 2003). "Epidemiology and aetiology of gestational trophoblastic diseases". The Lancet. Oncology. 4 (11): 670–678. doi:10.1016/S1470-2045(03)01245-2. PMID 14602247.
- 1 2 3 Steigrad SJ (December 2003). "Epidemiology of gestational trophoblastic diseases". Best Practice & Research. Clinical Obstetrics & Gynaecology. 17 (6): 837–847. doi:10.1016/s1521-6934(03)00049-x. PMID 14614884.
- ↑ Silva AL, Monteiro KD, Sun SY, Borbely AU (December 2021). "Gestational trophoblastic neoplasia: Novelties and challenges". Placenta. Trophoblast Research - Volume 39. 116: 38–42. doi: 10.1016/j.placenta.2021.02.013 . PMID 33685753. S2CID 232161179.
- 1 2 3 4 Di Fiore R, Suleiman S, Felix A, O'Toole SA, O'Leary JJ, Ward MP, et al. (June 2021). "An Overview of the Role of Long Non-Coding RNAs in Human Choriocarcinoma". International Journal of Molecular Sciences. 22 (12): 6506. doi: 10.3390/ijms22126506 . PMC 8235025 . PMID 34204445.
- ↑ Buza N (June 2022). "Gestational Trophoblastic Disease: Contemporary Diagnostic Approach". Surgical Pathology Clinics. 15 (2): 197–218. doi:10.1016/j.path.2022.02.002. PMID 35715158. S2CID 248959673.
- 1 2 Serno J, Zeppernick F, Jäkel J, Schrading S, Maass N, Meinhold-Heerlein I, Bauerschlag DO (2012). "Primary pulmonary choriocarcinoma: case report and review of the literature". Gynecologic and Obstetric Investigation. 74 (2): 171–176. doi:10.1159/000336784. PMID 22738859. S2CID 27897722.
- ↑ Mangla M, Singla D, Kaur H, Sharma S (February 2017). "Unusual clinical presentations of choriocarcinoma: A systematic review of case reports". Taiwanese Journal of Obstetrics & Gynecology. 56 (1): 1–8. doi: 10.1016/j.tjog.2015.05.011 . PMID 28254207.
- ↑ Buza N, Hui P (September 2021). "Genotyping diagnosis of gestational trophoblastic disease: frontiers in precision medicine". Modern Pathology. 34 (9): 1658–1672. doi: 10.1038/s41379-021-00831-9 . PMID 34088998.
- 1 2 3 4 5 6 Clark JJ, Slater S, Seckl MJ (February 2021). "Treatment of gestational trophoblastic disease in the 2020s". Current Opinion in Obstetrics & Gynecology. 33 (1): 7–12. doi:10.1097/GCO.0000000000000674. PMC 7116872 . PMID 33337613.
- 1 2 3 Lurain JR, Nejad B (May 2005). "Secondary chemotherapy for high-risk gestational trophoblastic neoplasia". Gynecologic Oncology. 97 (2): 618–623. doi: 10.1016/j.ygyno.2005.02.004 . PMID 15863169.
- 1 2 3 4 5 Winter MC (July 2021). "Treatment of low-risk gestational trophoblastic neoplasia". Best Practice & Research. Clinical Obstetrics & Gynaecology. 74: 67–80. doi:10.1016/j.bpobgyn.2021.01.006. PMID 33741258. S2CID 232302437.