The Puerto Rico Health Reform —Spanish: Reforma de Salud de Puerto Rico, refers to the Medicaid health plan which is a "subset of the larger public government healthcare delivery system" of Puerto Rico. It was once called "La Reforma", later it was called "Mi Salud" and now called Vital but they are all Medicaid, a government-run program which provides medical and healthcare services to indigent and impoverished citizens of Puerto Rico. It was locally referred to simply as La Reforma — for many years. Puerto Rico's Medicaid program is, similar to other Medicaid programs of states of the United States. The funding is by the U.S. Medicaid program in the form of a block grant, unlike how states of the United States Medicaid programs are funded and in 2019 much of the funding was slashed.

Healthcare in Mexico is provided by public institutions run by government departments, private hospitals and clinics, and private physicians. It is largely characterized by a special combination of coverage mainly based on the employment status of the people. Every Mexican citizen is guaranteed no cost access to healthcare and medicine according to the Mexican constitution and made a reality with the “Institute of Health for Well-being”, or INSABI.

Health care in Colombia refers to the prevention, treatment, and management of illness and the preservation of mental and physical well-being through the services offered by the medical, nursing, and allied health professions in the Republic of Colombia.

Healthcare in Singapore is under the purview of the Ministry of Health of the Government of Singapore. It mainly consists of a government-run publicly funded universal healthcare system as well as a significant private healthcare sector. Financing of healthcare costs is done through a mixture of direct government subsidies, compulsory comprehensive savings, national healthcare insurance, and cost-sharing.

Germany has a universal multi-payer health care system paid for by a combination of statutory health insurance and private health insurance.
The French health care system is one of universal health care largely financed by government national health insurance. In its 2000 assessment of world health care systems, the World Health Organization found that France provided the "best overall health care" in the world. In 2017, France spent 11.3% of GDP on health care, or US$5,370 per capita, a figure higher than the average spent by rich countries, though similar to Germany (10.6%) and Canada (10%), but much less than in the US. Approximately 77% of health expenditures are covered by government funded agencies.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).

Tanzania has a hierarchical health system which is in tandem with the political-administrative hierarchy. At the bottom, there are the dispensaries found in every village where the village leaders have a direct influence on its running. The health centers are found at ward level and the health center in charge is answerable to the ward leaders. At the district, there is a district hospital and at the regional level a regional referral hospital. The tertiary level is usually the zone hospitals and at a national level, there is the national hospital. There are also some specialized hospitals that do not fit directly into this hierarchy and therefore are directly linked to the ministry of health.

The Ministry of Health and Medical Education (MOHME) has executive responsibility for health and medical education within the Iranian government. The MOHME comprises five departments headed by deputy ministers: Health, Research & Technology, Education, Logistics, Food & Drugs.

Healthcare in Portugal is provided through three coexisting systems: the National Health Service, special social health insurance schemes for certain professions and voluntary private health insurance. The SNS provides universal coverage, although in 2012 measures were implemented to ensure the sustainability of the service by the introduction of user fees to be paid for at the end of treatments. In addition, about 25% of the population is covered by the health subsystems, 10% by private insurance schemes and another 7% by mutual funds. The Ministry of Health is responsible for developing health policy as well as managing the SNS. The Health Regulatory Entity (ERS) is the public independent entity responsible for the regulation of the activity of all the public, private and social healthcare providers. In 2019 the government proposes to scrap all fees, which constitute about 2 percent of the NHS's budget, apart from some hospital emergencies.
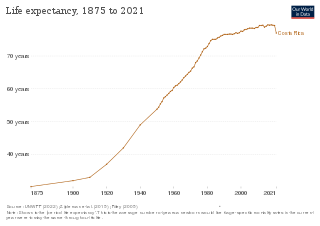
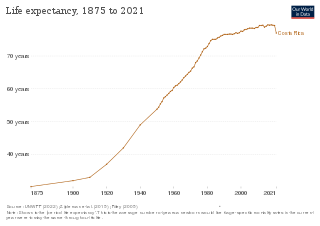
Costa Rica provides universal health care to its citizens and permanent residents. Both the private and public health care systems in Costa Rica are continually being upgraded. Statistics from the World Health Organization (WHO) frequently place Costa Rica in the top country rankings in the world for long life expectancy. WHO's 2000 survey ranked Costa Rica as having the 36th best health care system, placing it one spot above the United States at the time. In addition, the UN has ranked Costa Rica's public health system within the top 20 worldwide and the number 1 in Latin America.

The healthcare system in Chile is a mixed system that combines both public and private provision of health services. The public system is called Fondo Nacional de Salud (FONASA) and is funded by taxes, providing free or subsidized care for those who cannot afford private health insurance. The private system is composed of various insurance providers (ISAPRE) and healthcare facilities, which offer more extensive services to those who can afford to pay.

Healthcare in Belgium is composed of three parts. Firstly there is a primarily publicly funded healthcare and social security service run by the federal government, which organises and regulates healthcare; independent private/public practitioners, university/semi-private hospitals and care institutions. There are a few private hospitals. Secondly is the insurance coverage provided for patients. Finally, industry coverage; which covers the production and distribution of healthcare products for research and development. The primary aspect of this research is done in universities and hospitals.

Rashtriya Swasthya Bima Yojana is a government-run health insurance programme for the Indian poor. The scheme aims to provide health insurance coverage to the unrecognised sector workers belonging to the BPL category and their family members shall be beneficiaries under this scheme. It provides for cashless insurance for hospitalisation in public as well as private hospitals. The scheme started enrolling on April 1, 2008 and has been implemented in 25 states of India. A total of 36 million families have been enrolled as of February 2014. Initially, RSBY was a project under the Ministry of Labour and Employment. Now it has been transferred to Ministry of Health and Family Welfare from April 1, 2015
Examples of health care systems of the world, sorted by continent, are as follows.

Healthcare in Luxembourg is based on three fundamental principles: compulsory health insurance, free choice of healthcare provider for patients and compulsory compliance of providers in the set fixed costs for the services rendered. Citizens are covered by a healthcare system that provides medical, maternity and illness benefits and, for the elderly, attendance benefits. The extent of the coverage varies depending on the occupation of the individual. Those employed or receiving social security have full insurance coverage, and the self-employed and tradesmen are provided with both medical benefits and attendance benefits. That is all funded by taxes on citizens' incomes, payrolls and wages. However, the government covers the funding for maternity benefits as well as any other sector that needs additional funding. About 75% of the population purchases a complementary healthcare plan. About 99% of the people are covered under the state healthcare system.

Peru has a decentralized healthcare system that consists of a combination of governmental and non-governmental coverage. Five sectors administer healthcare in Peru today: the Ministry of Health, EsSalud, and the Armed Forces (FFAA), National Police (PNP), and the private sector.

The Egyptian healthcare system is pluralistic, comprising a variety of healthcare providers from the public as well as the private sector. The government ensures basic universal health coverage, although private services are also available for those with the ability to pay. Due to social and economic pressures, Egypt's healthcare system is subject to many challenges. However, several recent efforts have been directed towards enhancing the system.

The Ministry of Health of Argentina is a ministry of the national executive power that oversees, elaborates and coordinates the Argentine national state's public health policy. The ministry is responsible for overseeing Argentina's highly decentralized universal health care system, which according to 2000 figures, serviced over half of the country's population.