Carpal tunnel syndrome (CTS) is the collection of symptoms and signs associated with nerve compression of the median nerve at the carpal tunnel. Most CTS is related to idiopathic compression of the median nerve as it travels through the wrist at the carpal tunnel. Idiopathic means that there is no other disease process contributing to pressure on the nerve. As with most structural issues, it occurs in both hands, and the strongest risk factor is genetics.

The radial nerve is a nerve in the human body that supplies the posterior portion of the upper limb. It innervates the medial and lateral heads of the triceps brachii muscle of the arm, as well as all 12 muscles in the posterior osteofascial compartment of the forearm and the associated joints and overlying skin.

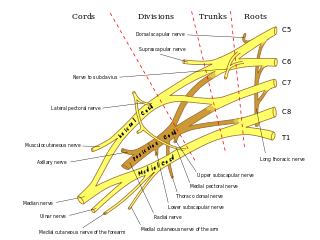
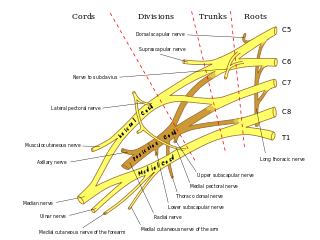
The median nerve is a nerve in humans and other animals in the upper limb. It is one of the five main nerves originating from the brachial plexus.
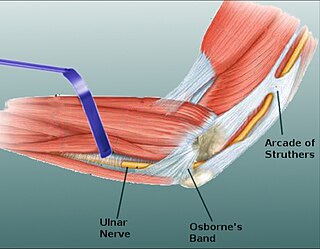
In human anatomy, the ulnar nerve is a nerve that runs near the ulna bone. The ulnar collateral ligament of elbow joint is in relation with the ulnar nerve. The nerve is the largest in the human body unprotected by muscle or bone, so injury is common. This nerve is directly connected to the little finger, and the adjacent half of the ring finger, innervating the palmar aspect of these fingers, including both front and back of the tips, perhaps as far back as the fingernail beds.

Wrist drop is a medical condition in which the wrist and the fingers cannot extend at the metacarpophalangeal joints. The wrist remains partially flexed due to an opposing action of flexor muscles of the forearm. As a result, the extensor muscles in the posterior compartment remain paralyzed.
The pronator teres is a muscle that, along with the pronator quadratus, serves to pronate the forearm. It has two origins, at the medial humeral supracondylar ridge and the ulnar tuberosity, and inserts near the middle of the radius.

The flexor retinaculum is a fibrous band on the palmar side of the hand near the wrist. It arches over the carpal bones of the hands, covering them and forming the carpal tunnel.

The ulnar canal or ulnar tunnel (also known as Guyon's canal or tunnel) is a semi-rigid longitudinal canal in the wrist that allows passage of the ulnar artery and ulnar nerve into the hand. The roof of the canal is made up of the superficial palmar carpal ligament, while the deeper flexor retinaculum and hypothenar muscles comprise the floor. The space is medially bounded by the pisiform and pisohamate ligament more proximally, and laterally bounded by the hook of the hamate more distally. It is approximately 4 cm long, beginning proximally at the transverse carpal ligament and ending at the aponeurotic arch of the hypothenar muscles.

The anterior interosseous nerve is a branch of the median nerve that supplies the deep muscles on the anterior of the forearm, except the ulnar (medial) half of the flexor digitorum profundus. Its nerve roots come from C8 and T1.

Ulnar tunnel syndrome, also known as Guyon's canal syndrome or Handlebar palsy, is ulnar neuropathy at the wrist where it passes through the Guyon canal. The most common presentation is a palsy of the deep motor branch of the ulnar nerve causing weakness of the interosseous muscles. Many are associated with a ganglion cyst pressing on the ulnar nerve, but most are idiopathic. Long distance bicycle rides are associated with transient alterations in ulnar nerve function. Sensory loss in the ring and small fingers is usually due to ulnar nerve entrapment at the cubital tunnel near the elbow, which is known as cubital tunnel syndrome, although it can uncommonly be due to compression at the wrist.

In the human body, the carpal tunnel or carpal canal is a flattened body cavity on the flexor (palmar/volar) side of the wrist, bounded by the carpal bones and flexor retinaculum. It forms the passageway that transmits the median nerve and the tendons of the extrinsic flexor muscles of the hand from the forearm to the hand. There are described cases of the anatomical variant median artery occurrence.

Ulnar neuropathy is a disorder involving the ulnar nerve. Ulnar neuropathy may be caused by entrapment of the ulnar nerve with resultant numbness and tingling. It may also cause weakness or paralysis of the muscles supplied by the nerve.

The elbow is the region between the upper arm and the forearm that surrounds the elbow joint. The elbow includes prominent landmarks such as the olecranon, the cubital fossa, and the lateral and the medial epicondyles of the humerus. The elbow joint is a hinge joint between the arm and the forearm; more specifically between the humerus in the upper arm and the radius and ulna in the forearm which allows the forearm and hand to be moved towards and away from the body. The term elbow is specifically used for humans and other primates, and in other vertebrates it is not used. In those cases, forelimb plus joint is used.
Anterior interosseous syndrome is a medical condition in which damage to the anterior interosseous nerve (AIN), a distal motor and sensory branch of the median nerve, classically with severe weakness of the pincer movement of the thumb and index finger, and can cause transient pain in the wrist.

Pronator teres syndrome is a compression neuropathy of the median nerve at the elbow. It is rare compared to compression at the wrist or isolated injury of the anterior interosseous branch of the median nerve.
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi.

Injuries to the arm, forearm or wrist area can lead to various nerve disorders. One such disorder is median nerve palsy. The median nerve controls the majority of the muscles in the forearm. It controls abduction of the thumb, flexion of hand at wrist, flexion of digital phalanx of the fingers, is the sensory nerve for the first three fingers, etc. Because of this major role of the median nerve, it is also called the eye of the hand. If the median nerve is damaged, the ability to abduct and oppose the thumb may be lost due to paralysis of the thenar muscles. Various other symptoms can occur which may be repaired through surgery and tendon transfers. Tendon transfers have been very successful in restoring motor function and improving functional outcomes in patients with median nerve palsy.

Radial nerve dysfunction is a problem associated with the radial nerve resulting from injury consisting of acute trauma to the radial nerve. The damage has sensory consequences, as it interferes with the radial nerve's innervation of the skin of the posterior forearm, lateral three digits, and the dorsal surface of the lateral side of the palm. The damage also has motor consequences, as it interferes with the radial nerve's innervation of the muscles associated with the extension at the elbow, wrist, and fingers, as well the supination of the forearm. This type of injury can be difficult to localize, but relatively common, as many ordinary occurrences can lead to the injury and resulting mononeuropathy. One out of every ten patients with radial nerve dysfunction do so because of a fractured humerus.
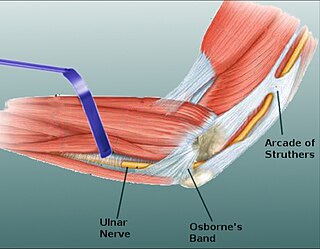
Osborne's ligament, also Osborne's band, Osborne's fascia, Osborne's arcade, arcuate ligament of Osborne, or the cubital tunnel retinaculum, refers to either the connective tissue which spans the humeral and ulnar heads of the flexor carpi ulnaris (FCU) or another distinct tissue located between the olecranon process of the ulna and the medial epicondyle of the humerus. It is named after Geoffrey Vaughan Osborne, a British orthopedic surgeon, who described the eponymous tissue in 1957.
Nerve glide, also known as nerve flossing or nerve stretching, is an exercise that stretches nerves. It facilitates the smooth and regular movement of peripheral nerves in the body. It allows the nerve to glide freely along with the movement of the joint and relax the nerve from compression. Nerve gliding cannot proceed with injuries or inflammations as the nerve is trapped by the tissue surrounding the nerve near the joint. Thus, nerve gliding exercise is widely used in rehabilitation programs and during the post-surgical period.