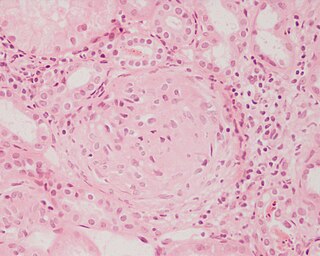
Inflammation is part of the biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a protective response involving immune cells, blood vessels, and molecular mediators. The function of inflammation is to eliminate the initial cause of cell injury, clear out damaged cells and tissues, and initiate tissue repair.
Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition involving a severe and dangerous lowered white blood cell count and thus causing neutropenia in the circulating blood. It is a severe lack of one major class of infection-fighting white blood cells. People with this condition are at very high risk of serious infections due to their suppressed immune system.
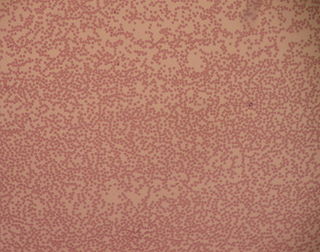
Neutropenia is an abnormally low concentration of neutrophils in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria, bacterial fragments and immunoglobulin-bound viruses in the blood. People with neutropenia are more susceptible to bacterial infections and, without prompt medical attention, the condition may become life-threatening.

Neutrophiliaa is leukocytosis of neutrophils, that is, a high number of neutrophils in the blood. Because neutrophils are the main type of granulocytes, mentions of granulocytosis often overlap in meaning with neutrophilia.
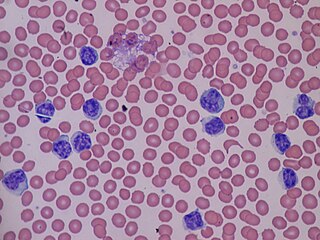
Lymphocytosis is an increase in the number or proportion of lymphocytes in the blood. Absolute lymphocytosis is the condition where there is an increase in the lymphocyte count beyond the normal range while relative lymphocytosis refers to the condition where the proportion of lymphocytes relative to white blood cell count is above the normal range. In adults, absolute lymphocytosis is present when the lymphocyte count is greater than 5000 per microliter (5.0 x 109/L), in older children greater than 7000 per microliter and in infants greater than 9000 per microliter. Lymphocytes normally represent 20% to 40% of circulating white blood cells. When the percentage of lymphocytes exceeds 40%, it is recognized as relative lymphocytosis.
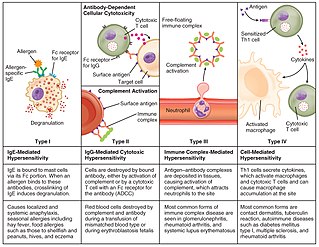
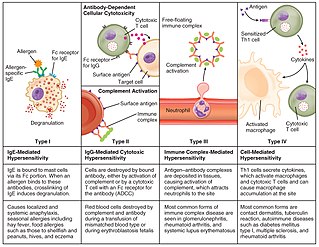
Hypersensitivity is an abnormal physiological condition in which there is an undesirable and adverse immune response to antigen. It is an abnormality in the immune system that causes immune diseases including allergies and autoimmunity. It is caused by many types of particles and substances from the external environment or from within the body that are recognized by the immune cells as antigens. The immune reactions are usually referred to as an over-reaction of the immune system and they are often damaging and uncomfortable.

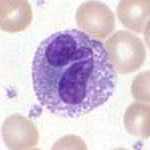
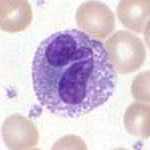
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and monocyte-derived dendritic cells. As a part of the vertebrate innate immune system monocytes also influence adaptive immune responses and exert tissue repair functions. There are at least three subclasses of monocytes in human blood based on their phenotypic receptors.
Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear, that is, they have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.
Leukocytosis is a condition in which the white cell (leukocyte) count is above the normal range in the blood. It is frequently a sign of an inflammatory response, most commonly the result of infection, but may also occur following certain parasitic infections or bone tumors as well as leukemia. It may also occur after strenuous exercise, convulsions such as epilepsy, emotional stress, pregnancy and labor, anesthesia, as a side effect of medication, and epinephrine administration. There are five principal types of leukocytosis:
- Neutrophilia
- Lymphocytosis
- Monocytosis
- Eosinophilia
- Basophilia
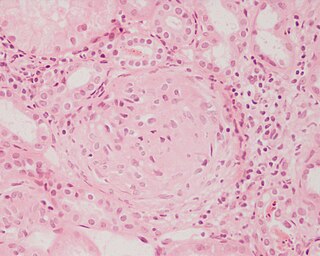
Glomerulonephritis (GN) is a term used to refer to several kidney diseases. Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the name, but not all diseases necessarily have an inflammatory component.
Leukapheresis is a laboratory procedure in which white blood cells are separated from a sample of blood. It is a specific type of apheresis, the more general term for separating out one particular constituent of blood and returning the remainder to the circulation.
Fever of unknown origin (FUO) refers to a condition in which the patient has an elevated temperature (fever) but, despite investigations by one or more qualified physicians, no explanation is found.
Felty's syndrome (FS), also called Felty syndrome, is a rare autoimmune disease characterized by the triad of rheumatoid arthritis, enlargement of the spleen and low neutrophil count. The condition is more common in those aged 50–70 years, specifically more prevalent in females than males, and more so in Caucasians than those of African descent. It is a deforming disease that causes many complications for the individual.
Febrile neutropenia is the development of fever, often with other signs of infection, in a patient with neutropenia, an abnormally low number of neutrophil granulocytes in the blood. It is an oncologic emergency, and is the most common serious complication in patients with hematopoietic cancers or receiving chemotherapy for cancer. The term neutropenic sepsis is also applied, although it tends to be reserved for patients who are less well. In 50% of cases, an infection is detectable; bacteremia is present in approximately 20% of all patients with this condition.

Basophilia is the condition of having greater than 200 basophils/μL in the venous blood. Basophils are the least numerous of the myelogenous cells, and it is rare for their numbers to be abnormally high without changes to other blood components. Rather, basophilia is most often coupled with other white blood cell conditions such as eosinophilia, high levels of eosinophils in the blood. Basophils are easily identifiable by a blue coloration of the granules within each cell, marking them as granulocytes, in addition to segmented nuclei.
Monocytopenia is a form of leukopenia associated with a deficiency of monocytes.

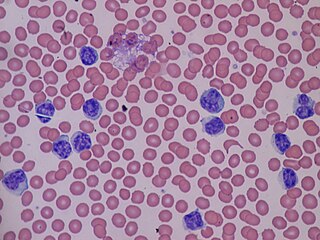
White blood cells, also called leukocytes, immune cells, or immunocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. White blood cells include three main subtypes; granulocytes, lymphocytes and monocytes.

Lymphocytic pleocytosis is an abnormal increase in the amount of lymphocytes in the cerebrospinal fluid (CSF). It is usually considered to be a sign of infection or inflammation within the nervous system, and is encountered in a number of neurological diseases, such as pseudomigraine, Susac's syndrome, and encephalitis. While lymphocytes make up roughly a quarter of all white blood cells (WBC) in the body, they are generally rare in the CSF. Under normal conditions, there are usually less than 5 white blood cells per µL of CSF. In a pleocytic setting, the number of lymphocytes can jump to more than 1,000 cells per µL. Increases in lymphocyte count are often accompanied by an increase in cerebrospinal protein concentrations in addition to pleocytosis of other types of white blood cells.

Toxic vacuolation, also known as toxic vacuolization, is the formation of vacuoles in the cytoplasm of neutrophils in response to severe infections or inflammatory conditions.

A white blood cell differential is a medical laboratory test that provides information about the types and amounts of white blood cells in a person's blood. The test, which is usually ordered as part of a complete blood count (CBC), measures the amounts of the five normal white blood cell types – neutrophils, lymphocytes, monocytes, eosinophils and basophils – as well as abnormal cell types if they are present. These results are reported as percentages and absolute values, and compared against reference ranges to determine whether the values are normal, low, or high. Changes in the amounts of white blood cells can aid in the diagnosis of many health conditions, including viral, bacterial, and parasitic infections and blood disorders such as leukemia.