Related Research Articles

Clozapine is a psychiatric medication and was the first atypical antipsychotic to be discovered. It is primarily used to treat people with schizophrenia and schizoaffective disorder who have had an inadequate response to two other antipsychotics, or who have been unable to tolerate other drugs due to extrapyramidal side effects. It is also used for the treatment of psychosis in Parkinson's disease.
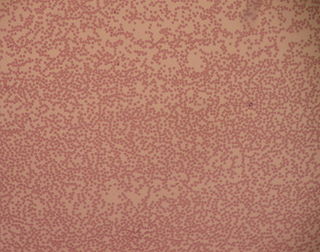
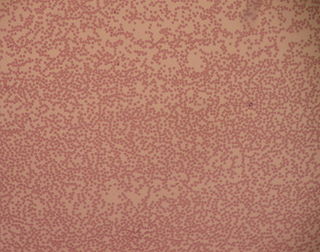
Neutropenia is an abnormally low concentration of neutrophils in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria, bacterial fragments and immunoglobulin-bound viruses in the blood. People with neutropenia are more susceptible to bacterial infections and, without prompt medical attention, the condition may become life-threatening.

Neutrophilia is leukocytosis of neutrophils, that is, a high number of neutrophils in the blood. Because neutrophils are the main type of granulocytes, mentions of granulocytosis often overlap in meaning with neutrophilia.

Granulocyte colony-stimulating factor, also known as colony-stimulating factor 3, is a glycoprotein that stimulates the bone marrow to produce granulocytes and stem cells and release them into the bloodstream.

Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear, that is, they have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.

Leukopenia is a decrease in the number of leukocytes (WBC). Found in the blood, they are the white blood cells, and are the body's primary defense against an infection. Thus the condition of leukopenia places individuals at increased risk of infection.
Absolute neutrophil count (ANC) is a measure of the number of neutrophil granulocytes present in the blood. Neutrophils are a type of white blood cell that fights against infection.
Cytopenia is a reduction in the number of mature blood cells. It can have many causes, and commonly occurs in people with cancer being treated with radiation therapy or chemotherapy.
Myelokathexis is a congenital disorder of the white blood cells that causes severe, chronic leukopenia and neutropenia. The disorder is believed to be inherited in an autosomal dominant manner. Myelokathexis refers to retention (kathexis) of neutrophils in the bone marrow (myelo). The disorder shows prominent neutrophil morphologic abnormalities.
Cyclic neutropenia (CyN) is a rare hematologic disorder and form of congenital neutropenia that tends to occur approximately every three weeks and lasting for few days at a time due to changing rates of neutrophil production by the bone marrow. It causes a temporary condition with a low absolute neutrophil count and because the neutrophils make up the majority of circulating white blood cells it places the body at severe risk of inflammation and infection. In comparison to severe congenital neutropenia, it responds well to treatment with granulocyte colony-stimulating factor (filgrastim), which increases the neutrophil count, shortens the cycle length, as well decreases the severity and frequency of infections.
Severe congenital neutropenia (SCN), also often known as Kostmann syndrome or disease, is a group of rare disorders that affect myelopoiesis, causing a congenital form of neutropenia, usually without other physical malformations. SCN manifests in infancy with life-threatening bacterial infections. It causes severe pyogenic infections. It can be caused by autosomal dominant inheritance of the ELANE gene, autosomal recessive inheritance of the HAX1 gene. There is an increased risk of leukemia and myelodysplastic cancers.

A promyelocyte is a granulocyte precursor, developing from the myeloblast and developing into the myelocyte. Promyelocytes measure 12–20 microns in diameter. The nucleus of a promyelocyte is approximately the same size as a myeloblast but their cytoplasm is much more abundant. They also have less prominent nucleoli than myeloblasts and their chromatin is more coarse and clumped. The cytoplasm is basophilic and contains primary red/purple granules.
Febrile neutropenia is the development of fever, often with other signs of infection, in a patient with neutropenia, an abnormally low number of neutrophil granulocytes in the blood. It is an oncologic emergency, and is the most common serious complication in patients with hematopoietic cancers or receiving chemotherapy for cancer. The term neutropenic sepsis is also applied, although it tends to be reserved for patients who are less well. In 50% of cases, an infection is detectable; bacteremia is present in approximately 20% of all patients with this condition.
Autoimmune neutropenia (AIN) is a form of neutropenia which is most common in infants and young children where the body identifies the neutrophils as enemies and makes antibodies to destroy them.
In hematology, myelopoiesis in the broadest sense of the term is the production of bone marrow and of all cells that arise from it, namely, all blood cells. In a narrower sense, myelopoiesis also refers specifically to the regulated formation of myeloid leukocytes (myelocytes), including eosinophilic granulocytes, basophilic granulocytes, neutrophilic granulocytes, and monocytes.

White blood cells, also called immune cells or immunocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. White blood cells include three main subtypes: granulocytes, lymphocytes and monocytes.
Morning pseudoneutropenia is a transient reduction in the measured neutrophil count from peripheral samples. This is noticed in some patients who are taking antipsychotic medication. Morning pseudoneutropenia is thought to be due to diurnal variation in the amount of circulating white blood cells and changes in the levels of hematopoietic cytokines and granulocyte colony stimulating factor (GCSF). Antipsychotics may amplify the natural variation in these hematopoietic factors.
Levamisole induced necrosis syndrome (LINES) is a complication of adulterated cocaine recognized in 2011, caused by the use of levamisole as a cutting agent for cocaine. Spontaneous bruising of the earlobes is considered characteristic of this condition, but lesions can present anywhere on the body.

A white blood cell differential is a medical laboratory test that provides information about the types and amounts of white blood cells in a person's blood. The test, which is usually ordered as part of a complete blood count (CBC), measures the amounts of the five normal white blood cell types – neutrophils, lymphocytes, monocytes, eosinophils and basophils – as well as abnormal cell types if they are present. These results are reported as percentages and absolute values, and compared against reference ranges to determine whether the values are normal, low, or high. Changes in the amounts of white blood cells can aid in the diagnosis of many health conditions, including viral, bacterial, and parasitic infections and blood disorders such as leukemia.
A granulocyte transfusion is a medical procedure in which granulocytes are infused into a person's blood. Granulocyte transfusions were historically used to prevent and treat infections in people with neutropenia, but the practice declined in popularity in the 1980s. Interest in the procedure increased in the 1990s due to the development of more effective methods for harvesting granulocytes and a growing population of people with severe neutropenia from chemotherapy. However, the treatment's efficacy remains poorly understood and its use is controversial.
References
- ↑ Neutropenia at eMedicine
- ↑ Andersohn F, Konzen C, Garbe E (2007). "Systematic review: agranulocytosis induced by nonchemotherapy drugs". Ann. Intern. Med. 146 (9): 657–65. doi:10.7326/0003-4819-146-9-200705010-00009. PMID 17470834. S2CID 15585536.
- ↑ Vallerand, April Hazard (2014-06-05). Davis's drug guide for nurses. Sanoski, Cynthia A.,, Deglin, Judith Hopfer, 1950- (Fourteenth ed.). Philadelphia. ISBN 978-0-8036-4085-6. OCLC 881473728.
{{cite book}}: CS1 maint: location missing publisher (link) - ↑ Elisa Mari; Franco Ricci; Davide Imberti; Massimo Gallerani (June 2011). "Agranulocytosis: an adverse effect of allopurinol treatment". Italian Journal of Medicine. 5 (2): 120–3. doi: 10.1016/j.itjm.2011.02.006 .
- ↑ Diaz, Jaime (1996). How Drugs Influence Behavior. Englewood Cliffs: Prentice Hall. ISBN 978-0132815604.
- ↑ Mijovic A, MacCabe JH (November 2020). "Clozapine-induced agranulocytosis". Ann Hematol. 99 (11): 2477–2482. doi:10.1007/s00277-020-04215-y. PMC 7536144 . PMID 32815018.
- ↑ U.S. Department of Justice; National Drug Intelligence Center (February 2010). "Colombian Cocaine Producers Increase Use of a Harmful Cutting Agent". National Drug Threat Assessment 2010. Archived from the original on 2012-05-18. Retrieved 2020-11-22.
- ↑ Centers for Disease Control Prevention (CDC) (December 2009). "Agranulocytosis associated with cocaine use — four States, March 2008–November 2009". MMWR Morb. Mortal. Wkly. Rep. 58 (49): 1381–5. PMID 20019655. Archived from the original on 2018-10-09. Retrieved 2017-09-08. Cited in Hsu, Jeremy (18 December 2009). "Majority of U.S. Cocaine Supply Cut with Veterinary Deworming Drug". Popular Science. Archived from the original on 25 February 2018. Retrieved 21 December 2009.
- ↑ Kumar, Vinay (2007). Robbins Basic Pathology (8 ed.). Elsevier. p. 441.