Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, platelets, and other clotting factors.
Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition involving a severe and dangerous lowered white blood cell count and thus causing neutropenia in the circulating blood. It is a severe lack of one major class of infection-fighting white blood cells. People with this condition are at very high risk of serious infections due to their suppressed immune system.
Neutropenia is an abnormally low concentration of neutrophils in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria, bacterial fragments and immunoglobulin-bound viruses in the blood. People with neutropenia are more susceptible to bacterial infections and, without prompt medical attention, the condition may become life-threatening.

Neutrophilia is leukocytosis of neutrophils, that is, a high number of neutrophils in the blood. Because neutrophils are the main type of granulocytes, mentions of granulocytosis often overlap in meaning with neutrophilia.
Bone marrow suppression also known as myelotoxicity or myelosuppression, is the decrease in production of cells responsible for providing immunity (leukocytes), carrying oxygen (erythrocytes), and/or those responsible for normal blood clotting (thrombocytes). Bone marrow suppression is a serious side effect of chemotherapy and certain drugs affecting the immune system such as azathioprine. The risk is especially high in cytotoxic chemotherapy for leukemia.

Granulocyte colony-stimulating factor, also known as colony-stimulating factor 3, is a glycoprotein that stimulates the bone marrow to produce granulocytes and stem cells and release them into the bloodstream.
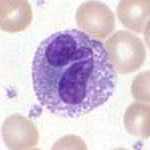
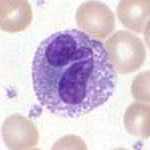
Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear. They have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.

Apheresis is a medical technology in which the blood of a person is passed through an apparatus that separates out one particular constituent and returns the remainder to the circulation. It is thus an extracorporeal therapy.

Leukopenia is a decrease in the number of leukocytes (WBC). Found in the blood, they are the white blood cells, and are the body's primary defense against an infection. Thus the condition of leukopenia places individuals at increased risk of infection.
Cytopenia is a reduction in the number of mature blood cells. It commonly occurs in people with cancer being treated with radiation therapy or chemotherapy.
Leukapheresis is a laboratory procedure in which white blood cells are separated from a sample of blood. It is a specific type of apheresis, the more general term for separating out one particular constituent of blood and returning the remainder to the circulation.
Cyclic neutropenia (CyN) is a rare hematologic disorder and form of congenital neutropenia that tends to occur approximately every three weeks and lasting for few days at a time due to changing rates of neutrophil production by the bone marrow. It causes a temporary condition with a low absolute neutrophil count and because the neutrophils make up the majority of circulating white blood cells it places the body at severe risk of inflammation and infection. In comparison to severe congenital neutropenia, it responds well to treatment with granulocyte colony-stimulating factor (filgrastim), which increases the neutrophil count, shortens the cycle length, as well decreases the severity and frequency of infections.

Fludarabine is a purine analogue and antineoplastic agent. It is generally used as its 5-O-phosphorylated form known as fludarabine phosphate, sold under the brand name Fludara among others. It is a chemotherapy medication used in the treatment of leukemia and lymphoma. These include chronic lymphocytic leukemia, non-Hodgkin's lymphoma, acute myeloid leukemia, and acute lymphocytic leukemia. It is given by injection into a vein or by mouth.

Sweet syndrome (SS), or acute febrile neutrophilic dermatosis, is a skin disease characterized by the sudden onset of fever, an elevated white blood cell count, and tender, red, well-demarcated papules and plaques that show dense infiltrates by neutrophil granulocytes on histologic examination.

Transfusion-related acute lung injury (TRALI) is the serious complication of transfusion of blood products that is characterized by the rapid onset of excess fluid in the lungs. It can cause dangerous drops in the supply of oxygen to body tissues. Although changes in transfusion practices have reduced the incidence of TRALI, it was the leading cause of transfusion-related deaths in the United States from fiscal year 2008 through fiscal year 2012.

WHIM syndrome is a rare congenital immunodeficiency disorder characterized by chronic noncyclic neutropenia.
Febrile neutropenia is the development of fever, often with other signs of infection, in a patient with neutropenia, an abnormally low number of neutrophil granulocytes in the blood. The term neutropenic sepsis is also applied, although it tends to be reserved for patients who are less well. In 50% of cases, an infection is detectable; bacteremia is present in approximately 20% of all patients with this condition.
Autoimmune neutropenia (AIN) is a form of neutropenia which is most common in infants and young children where the body identifies the neutrophils as enemies and makes antibodies to destroy them.

White blood cells, also called leukocytes or leucocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. White blood cells include three main subtypes; granulocytes, lymphocytes and monocytes.

Toxic vacuolation, also known as toxic vacuolization, is the formation of vacuoles in the cytoplasm of neutrophils in response to severe infections or inflammatory conditions.