A blood type is a classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system. Some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens can stem from one allele and collectively form a blood group system.

Blood transfusion is the process of transferring blood products into one's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, clotting factors, and platelets.

Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.
A Coombs test, also known as antiglobulin test (AGT) is either of two blood tests used in immunohematology. They are the direct and indirect Coombs tests. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells, a person can be anemic and this test can help clarify the condition. The indirect Coombs detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells and the test can be done to diagnose reactions to a blood transfusion.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, affecting one to three people per 100,000 per year. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
The Kidd antigen system are proteins found in the Kidd's blood group, which act as antigens, i.e., they have the ability to produce antibodies under certain circumstances. The Jk antigen is found on a protein responsible for urea transport in the red blood cells and the kidney. They are important in transfusion medicine. People with two Jk(a) antigens, for instance, may form antibodies against donated blood containing two Jk(b) antigens. This can lead to hemolytic anemia, in which the body destroys the transfused blood, leading to low red blood cell counts. Another disease associated with the Jk antigen is hemolytic disease of the newborn, in which a pregnant woman's body creates antibodies against the blood of her fetus, leading to destruction of the fetal blood cells. Hemolytic disease of the newborn associated with Jk antibodies is typically mild, though fatal cases have been reported.

The Colton antigen system (Co) is present on the membranes of red blood cells and in the tubules of the kidney and helps determine a person's blood type. The Co antigen is found on a protein called aquaporin-1 which is responsible for water homeostasis and urine concentration.
The Rh blood group system is a human blood group system. It contains proteins on the surface of red blood cells. It is the second most important blood group system, after the ABO blood group system. The Rh blood group system consists of 49 defined blood group antigens, among which the five antigens D, C, c, E, and e are the most important. There is no d antigen. Rh(D) status of an individual is normally described with a positive or negative suffix after the ABO type. The terms Rh factor, Rh positive, and Rh negative refer to the Rh(D) antigen only. Antibodies to Rh antigens can be involved in hemolytic transfusion reactions and antibodies to the Rh(D) and Rh antigens confer significant risk of hemolytic disease of the fetus and newborn.
The MNS antigen system is a human blood group system based upon two genes on chromosome 4. There are currently 50 antigens in the system, but the five most important are called M, N, S, s, and U.
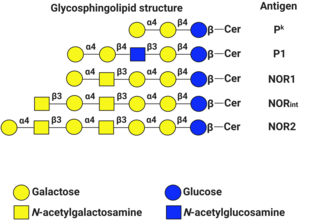
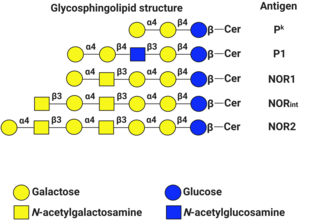
P1PK is a human blood group system based upon the A4GALT gene on chromosome 22. The P antigen was first described by Karl Landsteiner and Philip Levine in 1927. The P1PK blood group system consists of three glycosphingolipid antigens: Pk, P1 and NOR. In addition to glycosphingolipids, terminal Galα1→4Galβ structures are present on complex-type N-glycans. The GLOB antigen is now the member of the separate GLOB blood group system.
Packed red blood cells, also known as packed cells, are red blood cells that have been separated for blood transfusion. The packed cells are typically used in anemia that is either causing symptoms or when the hemoglobin is less than usually 70–80 g/L. In adults, one unit brings up hemoglobin levels by about 10 g/L. Repeated transfusions may be required in people receiving cancer chemotherapy or who have hemoglobin disorders. Cross matching is typically required before the blood is given. It is given by injection into a vein.
The LW blood system was first described by Landsteiner and Wiener in 1940. It was often confused with the Rh system, not becoming a separate antigen system until 1982. The LW and RhD antigens are genetically independent though they are phenotypically related and the LW antigen is expressed more strongly on RhD positive cells than on RhD negative cells. In most populations, the antithetical LW antigens, LWa and LWb are present as very high and very low frequency, respectively.
A delayed hemolytic transfusion reaction (DHTR) is a type of transfusion reaction. According to the Centers for Disease Control's (CDC) National Healthcare Safety Network's (NHSN) Hemovigilance Module, it is defined as:
The Vel blood group is a human blood group that has been implicated in hemolytic transfusion reactions. The blood group consists of a single antigen, the high-frequency Vel antigen, which is expressed on the surface of red blood cells. Individuals are typed as Vel-positive or Vel-negative depending on the presence of this antigen. The expression of the antigen in Vel-positive individuals is highly variable and can range from strong to weak. Individuals with the rare Vel-negative blood type develop anti-Vel antibodies when exposed to Vel-positive blood, which can cause transfusion reactions on subsequent exposures.
The Junior blood group system is a human blood group defined by the presence or absence of the Jr(a) antigen, a high-frequency antigen that is found on the red blood cells of most individuals. People with the rare Jr(a) negative blood type can develop anti-Jr(a) antibodies, which may cause transfusion reactions and hemolytic disease of the newborn on subsequent exposures. Jr(a) negative blood is most common in people of Japanese heritage.

Blood compatibility testing is conducted in a medical laboratory to identify potential incompatibilities between blood types in blood transfusion. It is also used to diagnose and prevent some complications of pregnancy that can occur when the baby has a different blood group from the mother. Blood compatibility testing includes blood typing, which detects the antigens on red blood cells that determine a person's blood type; testing for unexpected antibodies against blood group antigens ; and, in the case of blood transfusions, mixing the recipient's plasma with the donor's red blood cells to detect incompatibilities (crossmatching). Routine blood typing involves determining the ABO and RhD type, and involves both identification of ABO antigens on red blood cells and identification of ABO antibodies in the plasma. Other blood group antigens may be tested for in specific clinical situations.
The Lan blood group system is a human blood group defined by the presence or absence of the Lan antigen on a person's red blood cells. More than 99.9% of people are positive for the Lan antigen. Individuals with the rare Lan-negative blood type, which is a recessive trait, can produce an anti-Lan antibody when exposed to Lan-positive blood. Anti-Lan antibodies may cause transfusion reactions on subsequent exposures to Lan-positive blood, and have also been implicated in mild cases of hemolytic disease of the newborn. However, the clinical significance of the antibody is variable. The antigen was first described in 1961, and Lan was officially designated a blood group in 2012.
The Sid blood group system is a human blood group defined by the presence or absence of the Sd(a) antigen on a person's red blood cells. About 96% of people are positive for the Sd(a) antigen, which is inherited as a dominant trait. Among Sd(a) positive individuals, the expression of the antigen ranges from extremely weak to extremely strong. Very strong expression of the antigen is referred to as a Sd(a++) phenotype. In addition to being expressed on red blood cells, Sd(a) is secreted in bodily fluids such as saliva and breast milk, and is found in the highest concentrations in urine. Urine testing is considered the most reliable method for determining a person's Sid blood type.
The Augustine blood group system is a human blood group system. It includes four red blood cell surface glycoprotein antigens which are encoded by alleles of the gene SLC29A1.
The Er blood group collection is a collection of three human red blood cell surface antigens, Era, Erb, and Er3. The incidences of Era and Er3 are each greater than 99% of the human population, while the incidence of Erb is less than 0.01%. Individuals with antibodies against Er3 may develop acute hemolytic transfusion reaction upon transfusion with an incompatible unit, while Era and Erb are unlikely to be clinically significant.