Mechanical ventilation or assisted ventilation is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Extracorporeal membrane oxygenation (ECMO), is a form of extracorporeal life support, providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of oxygen, gas exchange or blood supply (perfusion) to sustain life. The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation. The device used is a membrane oxygenator, also known as an artificial lung.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.

Oxygen therapy, also referred to as supplemental oxygen, is the use of oxygen as medical treatment. Supplemental oxygen can also refer to the use of oxygen enriched air at altitude. Acute indications for therapy include hypoxemia, carbon monoxide toxicity and cluster headache. It may also be prophylactically given to maintain blood oxygen levels during the induction of anesthesia. Oxygen therapy is often useful in chronic hypoxemia caused by conditions such as severe COPD or cystic fibrosis. Oxygen can be delivered via nasal cannula, face mask, or endotracheal intubation at normal atmospheric pressure, or in a hyperbaric chamber. It can also be given through bypassing the airway, such as in ECMO therapy.

In medicine, a nebulizer or nebuliser is a drug delivery device used to administer medication in the form of a mist inhaled into the lungs. Nebulizers are commonly used for the treatment of asthma, cystic fibrosis, COPD and other respiratory diseases or disorders. They use oxygen, compressed air or ultrasonic power to break up solutions and suspensions into small aerosol droplets that are inhaled from the mouthpiece of the device. An aerosol is a mixture of gas and solid or liquid particles.

A breathing apparatus or breathing set is equipment which allows a person to breathe in a hostile environment where breathing would otherwise be impossible, difficult, harmful, or hazardous, or assists a person to breathe. A respirator, medical ventilator, or resuscitator may also be considered to be breathing apparatus. Equipment that supplies or recycles breathing gas other than ambient air in a space used by several people is usually referred to as being part of a life-support system, and a life-support system for one person may include breathing apparatus, when the breathing gas is specifically supplied to the user rather than to the enclosure in which the user is the occupant.

An oxygen mask is a mask that provides a method to transfer breathing oxygen gas from a storage tank to the lungs. Oxygen masks may cover only the nose and mouth or the entire face. They may be made of plastic, silicone, or rubber. In certain circumstances, oxygen may be delivered via a nasal cannula instead of a mask.
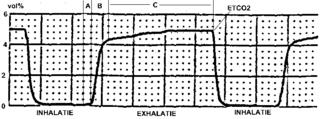
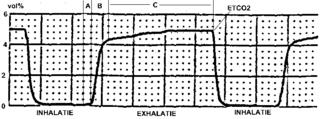
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO
2) in the respiratory gases. Its main development has been as a monitoring tool for use during anesthesia and intensive care. It is usually presented as a graph of CO
2 (measured in kilopascals, "kPa" or millimeters of mercury, "mmHg") plotted against time, or, less commonly, but more usefully, expired volume (known as volumetric capnography). The plot may also show the inspired CO
2, which is of interest when rebreathing systems are being used. When the measurement is taken at the end of a breath (exhaling), it is called "end tidal" CO
2 (PETCO2).

Alveolar lung diseases, are a group of diseases that mainly affect the alveoli of the lungs.
The venturi mask, also known as an air-entrainment mask, is a medical device to deliver a known oxygen concentration to patients on controlled oxygen therapy. The mask was invented by Moran Campbell at McMaster University Medical School as a replacement for intermittent oxygen treatment. Dr. Campbell was fond of quoting John Scott Haldane's description of intermittent oxygen treatment; "bringing a drowning man to the surface – occasionally". By contrast the venturi mask offered a constant supply of oxygen at a much more precise range of concentrations.

Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year.

The simple face mask (SFM) is a basic disposable mask, made of clear plastic, to provide oxygen therapy for patients who are experiencing conditions such as chest pain, dizziness, and minor hemorrhages. This mask is only meant for patients who are able to breathe on their own, but who may require a higher oxygen concentration than the 21% concentration found in ambient air. Patients who are unable to breathe on their own are placed on a medical ventilator instead. The simple face mask can deliver higher flow rates than nasal cannula for an FiO2 of 30- 60% oxygen. Nasal cannula and simple face masks are described as low flow delivery systems.

A non-rebreather mask is a device used in medicine to assist in the delivery of oxygen therapy. A NRB requires that the patient can breathe unassisted, but unlike a low-flow nasal cannula, the NRB allows for the delivery of higher concentrations of oxygen. An ideal non-rebreather mask does not permit air from the surrounding environment to be inhaled, hence an event of a source gas failure is life-threatening.
Respiratory gas humidification is a method of artificially conditioning respiratory gas for the patient during therapy, and involves humidification, warming, and occasionally filtration of the gas being delivered. If these three measures are not performed to compensate for the natural conditioning of air by the respiratory system, lung infections and lung tissue damage may occur. This is particularly problematic in high gas-flow therapies such as [mechanical ventilation], in patient populations with highly sensitive respiratory tracts, or among those requiring ventilation for longer periods of time. The two methods currently available for this purpose are active or passive respiratory gas humidification.

A portable oxygen concentrator (POC) is a device used to provide oxygen therapy to people that require greater oxygen concentrations than the levels of ambient air. It is similar to a home oxygen concentrator (OC), but is smaller in size and more mobile. They are small enough to carry and many are now FAA-approved for use on airplanes.

Heated humidified high-flow therapy, often simply called high flow therapy, is a type of respiratory support that delivers a flow of medical gas to a patient of up to 60 liters per minute and 100% oxygen through a large bore or high flow nasal cannula. Primarily studied in neonates, it has also been found effective in some adults to treat hypoxemia and work of breathing issues. The key components of it are a gas blender, heated humidifier, heated circuit, and cannula.
Vapotherm Inc. is a publicly held corporation based in Exeter, New Hampshire that was founded in 1999 as a medical device manufacturer after creating the first heated and humidified high flow therapy nasal cannula system.
Bubble CPAP is a non-invasive ventilation strategy for newborns with infant respiratory distress syndrome (IRDS). It is one of the methods by which continuous positive airway pressure (CPAP) is delivered to a spontaneously breathing newborn to maintain lung volumes during expiration. With this method, blended and humidified oxygen is delivered via short binasal prongs or a nasal mask and pressure in the circuit is maintained by immersing the distal end of the expiratory tubing in water. The depth to which the tubing is immersed underwater determines the pressure generated in the airways of the infant. As the gas flows through the system, it "bubbles" out and prevents buildup of excess pressures.
Demand Valve Oxygen Therapy (DVOT) is a way of delivering high flow oxygen therapy using a device that only delivers oxygen when the patient breathes in and shuts off when they breathe out. DVOT is commonly used to treat conditions such as cluster headache, which affects up to four in 1000 people (0.4%), and is a recommended first aid procedure for several diving disorders. It is also a recommended prophylactic for decompression sickness in the event of minor omitted decompression without symptoms.

A breathing apparatus or breathing set is equipment which allows a person to breathe in a hostile environment where breathing would otherwise be impossible, difficult, harmful, or hazardous, or assists a person to breathe. A respirator, medical ventilator, or resuscitator may also be considered to be breathing apparatus. Equipment that supplies or recycles breathing gas other than ambient air in a space used by several people is usually referred to as being part of a life-support system, and a life-support system for one person may include breathing apparatus, when the breathing gas is specifically supplied to the user rather than to the enclosure in which the user is the occupant.