Related Research Articles

Meconium aspiration syndrome (MAS) also known as neonatal aspiration of meconium is a medical condition affecting newborn infants. It describes the spectrum of disorders and pathophysiology of newborns born in meconium-stained amniotic fluid (MSAF) and have meconium within their lungs. Therefore, MAS has a wide range of severity depending on what conditions and complications develop after parturition. Furthermore, the pathophysiology of MAS is multifactorial and extremely complex which is why it is the leading cause of morbidity and mortality in term infants.

Mechanical ventilation or assisted ventilation is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.
Bronchiolitis is inflammation of the small airways in the lungs. Acute bronchiolitis is due to a viral infection usually affecting children younger than two years of age. Symptoms may include fever, cough, runny nose, wheezing, and breathing problems. More severe cases may be associated with nasal flaring, grunting, or the skin between the ribs pulling in with breathing. If the child has not been able to feed properly, signs of dehydration may be present.

Infant respiratory distress syndrome (IRDS), also called respiratory distress syndrome of newborn, or increasingly surfactant deficiency disorder (SDD), and previously called hyaline membrane disease (HMD), is a syndrome in premature infants caused by developmental insufficiency of pulmonary surfactant production and structural immaturity in the lungs. It can also be a consequence of neonatal infection and can result from a genetic problem with the production of surfactant-associated proteins.
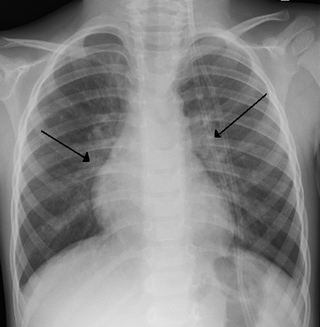
Transient tachypnea of the newborn is a respiratory problem that can be seen in the newborn shortly after delivery. It is caused by retained fetal lung fluid due to impaired clearance mechanisms. It is the most common cause of respiratory distress in term neonates. It consists of a period of tachypnea (rapid breathing. Usually, this condition resolves over 24–72 hours. Treatment is supportive and may include supplemental oxygen and antibiotics. The chest x-ray shows hyperinflation of the lungs including prominent pulmonary vascular markings, flattening of the diaphragm, and fluid in the horizontal fissure of the right lung.

A neonatal intensive care unit (NICU), also known as an intensive care nursery (ICN), is an intensive care unit (ICU) specializing in the care of ill or premature newborn infants. The NICU is divided into several areas, including a critical care area for babies who require close monitoring and intervention, an intermediate care area for infants who are stable but still require specialized care, and a step down unit where babies who are ready to leave the hospital can receive additional care before being discharged.

The nasal cannula (NC) is a device used to deliver supplemental oxygen or increased airflow to a patient or person in need of respiratory help. This device consists of a lightweight tube which on one end splits into two prongs which are placed in the nostrils curving toward the sinuses behind the nose, and from which a mixture of air and oxygen flows. The other end of the tube is connected to an oxygen supply such as a portable oxygen generator, or a wall connection in a hospital via a flowmeter. The cannula is generally attached to the patient by way of the tube hooking around the patient's ears or by an elastic headband, and the prongs curve toward the paranasal sinuses. The earliest, and most widely used form of adult nasal cannula carries 1–3 litres of oxygen per minute.

Bronchopulmonary dysplasia is a chronic lung disease which affects premature infants. Premature (preterm) infants who require treatment with supplemental oxygen or require long-term oxygen are at a higher risk. The alveoli that are present tend to not be mature enough to function normally. It is also more common in infants with low birth weight (LBW) and those who receive prolonged mechanical ventilation to treat respiratory distress syndrome. It results in significant morbidity and mortality. The definition of bronchopulmonary dysplasia has continued to evolve primarily due to changes in the population, such as more survivors at earlier gestational ages, and improved neonatal management including surfactant, antenatal glucocorticoid therapy, and less aggressive mechanical ventilation.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
Apnea of prematurity is a disorder in infants who are preterm that is defined as cessation of breathing by that lasts for more than 20 seconds and/or is accompanied by hypoxia or bradycardia. Apnea of prematurity is often linked to earlier prematurity. Apnea is traditionally classified as either obstructive, central, or mixed. Obstructive apnea may occur when the infant's neck is hyperflexed or conversely, hyperextended. It may also occur due to low pharyngeal muscle tone or to inflammation of the soft tissues, which can block the flow of air though the pharynx and vocal cords. Central apnea occurs when there is a lack of respiratory effort. This may result from central nervous system immaturity, or from the effects of medications or illness. Many episodes of apnea of prematurity may start as either obstructive or central, but then involve elements of both, becoming mixed in nature.

Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year.

Neonatal nursing is a sub-specialty of nursing care for newborn infants up to 28 days after birth. The term neonatal comes from neo, "new", and natal, "pertaining to birth or origin". Neonatal nursing requires a high degree of skill, dedication and emotional strength as they care for newborn infants with a range of problems. These problems vary between prematurity, birth defects, infection, cardiac malformations and surgical issues. Neonatal nurses are a vital part of the neonatal care team and are required to know basic newborn resuscitation, be able to control the newborn's temperature and know how to initiate cardiopulmonary and pulse oximetry monitoring. Most neonatal nurses care for infants from the time of birth until they are discharged from the hospital.
Fisher & Paykel Healthcare Corporation Limited (FPH) is a manufacturer, designer and marketer of products and systems for use in respiratory care, acute care, and the treatment of obstructive sleep apnea. Based in New Zealand, their products and systems are sold in around 120 countries worldwide. FPH is primarily an exporting company, with just 1 percent of revenue coming from New Zealand sales.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.

Heated humidified high-flow therapy, often simply called high flow therapy, is a type of respiratory support that delivers a flow of medical gas to a patient of up to 60 liters per minute and 100% oxygen through a large bore or high flow nasal cannula. Primarily studied in neonates, it has also been found effective in some adults to treat hypoxemia and work of breathing issues. The key components of it are a gas blender, heated humidifier, heated circuit, and cannula.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.

Henrik Verder is a pediatrician and the inventor of the INSURE and LISA methods combined with nasal CPAP. In 1989 he used this pioneering method to successfully treat the first premature infant with severe RDS. Verder is a significant researcher within the field of paediatrics, with more than 50 publications and over 500 citations.
Jen-Tien Wung is a Taiwanese-American pediatrician, author and professor of pediatrics at Columbia University's New York Presbyterian Hospital who developed Bubble CPAP for the treatment of premature babies.

A breathing apparatus or breathing set is equipment which allows a person to breathe in a hostile environment where breathing would otherwise be impossible, difficult, harmful, or hazardous, or assists a person to breathe. A respirator, medical ventilator, or resuscitator may also be considered to be breathing apparatus. Equipment that supplies or recycles breathing gas other than ambient air in a space used by several people is usually referred to as being part of a life-support system, and a life-support system for one person may include breathing apparatus, when the breathing gas is specifically supplied to the user rather than to the enclosure in which the user is the occupant.
References
- ↑ Morley CJ, Lau R, De Paoli A, Davis PG (July 2005). "Nasal continuous positive airway pressure: does bubbling improve gas exchange?". Archives of Disease in Childhood. Fetal and Neonatal Edition. 90 (4): F343-4. doi:10.1136/adc.2004.062588. PMC 1721902 . PMID 16036895.
- 1 2 3 Sahni R (February 2010). "Bubble CPAP: can we predict success or failure?". Indian Pediatrics. 47 (2): 129–30. doi: 10.1007/s13312-010-0019-0 . PMID 20228427.
- ↑ Dada S, Ashworth H, Sobitschka A, Raguveer V, Sharma R, Hamilton RL, Burke T (2021-06-11). "Experiences with implementation of continuous positive airway pressure for neonates and infants in low-resource settings: A scoping review". PLOS ONE. 16 (6): e0252718. Bibcode:2021PLoSO..1652718D. doi: 10.1371/journal.pone.0252718 . PMC 8195417 . PMID 34115776.
- ↑ Polin RA, Sahni R (October 2002). "Newer experience with CPAP". Seminars in Neonatology. 7 (5): 379–89. doi:10.1053/siny.2002.0132. PMID 12464500.
- ↑ Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK (June 1971). "Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure". The New England Journal of Medicine. 284 (24): 1333–40. doi:10.1056/NEJM197106172842401. PMID 4930602.
- 1 2 3 4 5 Chan SY, Chan CK, Hou SM, Ng C (2007). "The Use of Bubble CPAP in Premature Infants: Local experience" (PDF). Hong Kong Journal of Paediatrics. 12 (2): 86–92. doi: 10.1016/S1561-5413(08)60006-X .
- ↑ Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB, et al. (January 1987). "Is chronic lung disease in low birth weight infants preventable? A survey of eight centers". Pediatrics. 79 (1): 26–30. doi:10.1542/peds.79.1.26. PMID 3797169. S2CID 21853784.
- ↑ Narendran V, Donovan EF, Hoath SB, Akinbi HT, Steichen JJ, Jobe AH (Apr–May 2003). "Early bubble CPAP and outcomes in ELBW preterm infants". Journal of Perinatology. 23 (3): 195–9. doi:10.1038/sj.jp.7210904. PMID 12732855.
- 1 2 Fink, Sheri. Five Days at Memorial : Life and Death in a Storm-Ravaged Hospital. Atlantic Books, 2013.
- ↑ Won A, Suarez-Rebling D, Baker AL, Burke TF, Nelson BD (August 2019). "Bubble CPAP devices for infants and children in resource-limited settings: review of the literature". Paediatrics and International Child Health. 39 (3): 168–176. doi:10.1080/20469047.2018.1534389. PMID 30375281. S2CID 53113380.
- ↑ "Averting Newborn Deaths: Blending Oxygen and Bubble CPAP". Vayu Global Health Innovations.