| Iron lung | |
|---|---|
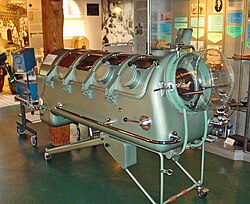
 An Emerson iron lung | |
| Specialty | Pulmonology |
| ICD-9-CM | 93.99 |
| MeSH | D015919 |
An iron lung is a type of negative pressure ventilator, a mechanical respirator which encloses most of a person's body and varies the air pressure in the enclosed space to stimulate breathing. [1] [2] It assists breathing when muscle control is lost, or the work of breathing exceeds the person's ability. [1] Need for this treatment may result from diseases including polio and botulism and certain poisons (for example, barbiturates and tubocurarine).
Contents
- Design and function
- Method and use
- Invention and early use
- Initial development
- Drinker and Shaw tank
- Both respirator
- Polio epidemic
- Outcomes
- Modern development and usage
- Replacement
- Continued use
- COVID-19 pandemic
- References
- Further reading
- External links
The use of iron lungs is largely obsolete in modern medicine as more modern breathing therapies have been developed [3] and due to the eradication of polio in most of the world. [4] In 2020, however, the COVID-19 pandemic revived some interest in them as a cheap, readily-producible substitute for positive-pressure ventilators, which were feared to be outnumbered by patients potentially needing temporary artificially assisted respiration. [5] [6] [7]
The iron lung is a large horizontal cylinder designed to stimulate breathing in patients who have lost control of their respiratory muscles. The patient's head is exposed outside the cylinder, while the body is sealed inside. Air pressure inside the cylinder is cycled to facilitate inhalation and exhalation. Devices like the Drinker, Emerson, and Both respirators are examples of iron lungs, which can be manually or mechanically powered. Smaller versions, like the cuirass ventilator and jacket ventilator, enclose only the patient's torso. Breathing in humans occurs through negative pressure, where the rib cage expands and the diaphragm contracts, causing air to flow in and out of the lungs.
The concept of external negative pressure ventilation was introduced by John Mayow in 1670. The first widely used device was the iron lung, developed by Philip Drinker and Louis Shaw in 1928. Initially used for coal gas poisoning treatment, the iron lung gained fame for treating respiratory failure caused by polio in the mid-20th century. John Haven Emerson introduced an improved and more affordable version in 1931. The Both respirator, a cheaper and lighter alternative to the Drinker model, was invented in Australia in 1937. British philanthropist William Morris financed the production of the Both–Nuffield respirators, donating them to hospitals throughout Britain and the British Empire. During the polio outbreaks of the 1940s and 1950s, iron lungs filled hospital wards, assisting patients with paralyzed diaphragms in their recovery.
Polio vaccination programs and the development of modern ventilators have nearly eradicated the use of iron lungs in the developed world. Positive pressure ventilation systems, which blow air into the patient's lungs via intubation, have become more common than negative pressure systems like iron lungs. However, negative pressure ventilation is more similar to normal physiological breathing and may be preferable in rare conditions such as central hypoventilation syndrome. [1] As of 2024 [update] , after the death of Paul Alexander, only one patient in the US, Martha Lillard, was still using an iron lung. [8] In response to the COVID-19 pandemic and the shortage of modern ventilators, some enterprises developed prototypes of new, easily producible versions of the iron lung.