First aid is the first and immediate assistance given to any person with either a minor or serious illness or injury, with care provided to preserve life, prevent the condition from worsening, or to promote recovery until medical services arrive. First aid is generally performed by someone with basic medical training. Mental health first aid is an extension of the concept of first aid to cover mental health, while psychological first aid is used as early treatment of people who are at risk for developing PTSD. Conflict first aid, focused on preservation and recovery of an individual's social or relationship well-being, is being piloted in Canada.

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.
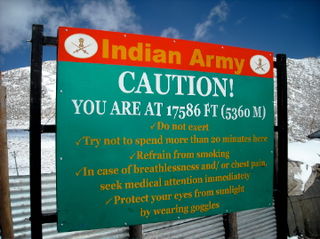
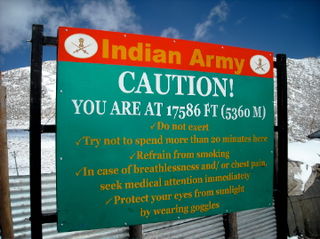
Altitude sickness, the mildest form being acute mountain sickness (AMS), is a harmful effect of high altitude, caused by rapid exposure to low amounts of oxygen at high elevation. People can respond to high altitude in different ways. Symptoms may include headaches, vomiting, tiredness, confusion, trouble sleeping, and dizziness. Acute mountain sickness can progress to high-altitude pulmonary edema (HAPE) with associated shortness of breath or high-altitude cerebral edema (HACE) with associated confusion. Chronic mountain sickness may occur after long-term exposure to high altitude.

Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered mental status due to ischemia in the brain.
Shortness of breath (SOB), also medically known as dyspnea or dyspnoea, is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity", and recommends evaluating dyspnea by assessing the intensity of its distinct sensations, the degree of distress and discomfort involved, and its burden or impact on the patient's activities of daily living. Distinct sensations include effort/work to breathe, chest tightness or pain, and "air hunger". The tripod position is often assumed to be a sign.

Mechanical ventilation or assisted ventilation is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Obesity hypoventilation syndrome (OHS) is a condition in which severely overweight people fail to breathe rapidly or deeply enough, resulting in low oxygen levels and high blood carbon dioxide (CO2) levels. The syndrome is often associated with obstructive sleep apnea (OSA), which causes periods of absent or reduced breathing in sleep, resulting in many partial awakenings during the night and sleepiness during the day. The disease puts strain on the heart, which may lead to heart failure and leg swelling.

Hyperbaric medicine is medical treatment in which an ambient pressure greater than sea level atmospheric pressure is a necessary component. The treatment comprises hyperbaric oxygen therapy (HBOT), the medical use of oxygen at an ambient pressure higher than atmospheric pressure, and therapeutic recompression for decompression illness, intended to reduce the injurious effects of systemic gas bubbles by physically reducing their size and providing improved conditions for elimination of bubbles and excess dissolved gas.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.

Oxygen therapy, also referred to as supplemental oxygen, is the use of oxygen as medical treatment. Supplemental oxygen can also refer to the use of oxygen enriched air at altitude. Acute indications for therapy include hypoxemia, carbon monoxide toxicity and cluster headache. It may also be prophylactically given to maintain blood oxygen levels during the induction of anesthesia. Oxygen therapy is often useful in chronic hypoxemia caused by conditions such as severe COPD or cystic fibrosis. Oxygen can be delivered via nasal cannula, face mask, or endotracheal intubation at normal atmospheric pressure, or in a hyperbaric chamber. It can also be given through bypassing the airway, such as in ECMO therapy.

A breathing apparatus or breathing set is equipment which allows a person to breathe in a hostile environment where breathing would otherwise be impossible, difficult, harmful, or hazardous, or assists a person to breathe. A respirator, medical ventilator, or resuscitator may also be considered to be breathing apparatus. Equipment that supplies or recycles breathing gas other than ambient air in a space used by several people is usually referred to as being part of a life-support system, and a life-support system for one person may include breathing apparatus, when the breathing gas is specifically supplied to the user rather than to the enclosure in which the user is the occupant.

An oxygen mask is a mask that provides a method to transfer breathing oxygen gas from a storage tank to the lungs. Oxygen masks may cover only the nose and mouth or the entire face. They may be made of plastic, silicone, or rubber. In certain circumstances, oxygen may be delivered via a nasal cannula instead of a mask.

The nasal cannula (NC) is a device used to deliver supplemental oxygen or increased airflow to a patient or person in need of respiratory help. This device consists of a lightweight tube which on one end splits into two prongs which are placed in the nostrils curving toward the sinuses behind the nose, and from which a mixture of air and oxygen flows. The other end of the tube is connected to an oxygen supply such as a portable oxygen generator, or a wall connection in a hospital via a flowmeter. The cannula is generally attached to the patient by way of the tube hooking around the patient's ears or by an elastic headband, and the prongs curve toward the paranasal sinuses. The earliest, and most widely used form of adult nasal cannula carries 1–3 litres of oxygen per minute.

High-altitude pulmonary edema (HAPE) is a life-threatening form of non-cardiogenic pulmonary edema that occurs in otherwise healthy people at altitudes typically above 2,500 meters (8,200 ft). However, cases have also been reported between 1,500–2,500 metres or 4,900–8,200 feet in more vulnerable subjects.
Hyperoxia occurs when cells, tissues and organs are exposed to an excess supply of oxygen (O2) or higher than normal partial pressure of oxygen.

Smoke inhalation is the breathing in of harmful fumes through the respiratory tract. This can cause smoke inhalation injury which is damage to the respiratory tract caused by chemical and/or heat exposure, as well as possible systemic toxicity after smoke inhalation. Smoke inhalation can occur from fires of various sources such as residential, vehicle, and wildfires. Morbidity and mortality rates in fire victims with burns are increased in those with smoke inhalation injury. Victims of smoke inhalation injury can present with cough, difficulty breathing, low oxygen saturation, smoke debris and/or burns on the face. Smoke inhalation injury can affect the upper respiratory tract, usually due to heat exposure, or the lower respiratory tract, usually due to exposure to toxic fumes. Initial treatment includes taking the victim away from the fire and smoke, giving 100% oxygen at a high flow through a face mask, and checking the victim for injuries to the body. Treatment for smoke inhalation injury is largely supportive, with varying degrees of consensus on benefits of specific treatments.

Acute decompensated heart failure (ADHF) is a sudden worsening of the signs and symptoms of heart failure, which typically includes difficulty breathing (dyspnea), leg or feet swelling, and fatigue. ADHF is a common and potentially serious cause of acute respiratory distress. The condition is caused by severe congestion of multiple organs by fluid that is inadequately circulated by the failing heart. An attack of decompensation can be caused by underlying medical illness, such as myocardial infarction, an abnormal heart rhythm, infection, or thyroid disease.

Oxygen saturation is the fraction of oxygen-saturated haemoglobin relative to total haemoglobin in the blood. The human body requires and regulates a very precise and specific balance of oxygen in the blood. Normal arterial blood oxygen saturation levels in humans are 97–100 percent. If the level is below 90 percent, it is considered low and called hypoxemia. Arterial blood oxygen levels below 80 percent may compromise organ function, such as the brain and heart, and should be promptly addressed. Continued low oxygen levels may lead to respiratory or cardiac arrest. Oxygen therapy may be used to assist in raising blood oxygen levels. Oxygenation occurs when oxygen molecules enter the tissues of the body. For example, blood is oxygenated in the lungs, where oxygen molecules travel from the air and into the blood. Oxygenation is commonly used to refer to medical oxygen saturation.
Demand Valve Oxygen Therapy (DVOT) is a way of delivering high flow oxygen therapy using a device that only delivers oxygen when the patient breathes in and shuts off when they breathe out. DVOT is commonly used to treat conditions such as cluster headache, which affects up to four in 1000 people (0.4%), and is a recommended first aid procedure for several diving disorders. It is also a recommended prophylactic for decompression sickness in the event of minor omitted decompression without symptoms.

A breathing apparatus or breathing set is equipment which allows a person to breathe in a hostile environment where breathing would otherwise be impossible, difficult, harmful, or hazardous, or assists a person to breathe. A respirator, medical ventilator, or resuscitator may also be considered to be breathing apparatus. Equipment that supplies or recycles breathing gas other than ambient air in a space used by several people is usually referred to as being part of a life-support system, and a life-support system for one person may include breathing apparatus, when the breathing gas is specifically supplied to the user rather than to the enclosure in which the user is the occupant.