Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.

Mechanical ventilation or assisted ventilation is the medical term for using a ventilator machine to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Laryngoscopy is endoscopy of the larynx, a part of the throat. It is a medical procedure that is used to obtain a view, for example, of the vocal folds and the glottis. Laryngoscopy may be performed to facilitate tracheal intubation during general anaesthesia or cardiopulmonary resuscitation or for surgical procedures on the larynx or other parts of the upper tracheobronchial tree.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients. Depending on the procedure, general anaesthesia may be optional or required. Regardless of whether a patient may prefer to be unconscious or not, certain pain stimuli could result in involuntary responses from the patient that may make an operation extremely difficult. Thus, for many procedures, general anaesthesia is required from a practical perspective.
A tracheal tube is a catheter that is inserted into the trachea for the primary purpose of establishing and maintaining a patent airway and to ensure the adequate exchange of oxygen and carbon dioxide.
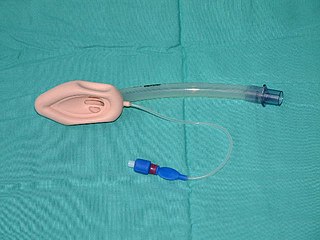
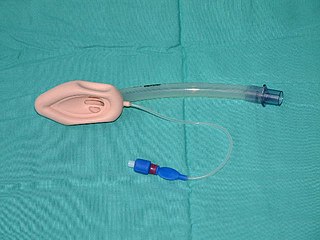
A laryngeal mask airway (LMA), also known as laryngeal mask, is a medical device that keeps a patient's airway open during anaesthesia or while they are unconscious. It is a type of supraglottic airway device. They are most commonly used by anaesthetists to channel oxygen or inhalational anaesthetic to the lungs during surgery and in the pre-hospital setting for unconscious patients.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).

Respiratory arrest is a serious medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.
In anaesthesia and advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.

In medicine, a nasopharyngeal airway (NPA), nasal trumpet, or nose hose, is a type of airway adjunct, a tube that is designed to be inserted through the nasal passage down into the posterior pharynx to secure an open airway. It was introduced by Hans Karl Wendl in 1958. When a patient becomes unconscious, the muscles in the jaw commonly relax and can allow the tongue to slide back and obstruct the airway. This makes airway management necessary, and an NPA is one of the available tools. The purpose of the flared end is to prevent the device from becoming lost inside the patient's nose.

A cricothyrotomy is an incision made through the skin and cricothyroid membrane to establish a patient airway during certain life-threatening situations, such as airway obstruction by a foreign body, angioedema, or massive facial trauma. Cricothyrotomy is nearly always performed as a last resort in cases where other means of tracheal intubation are impossible or impractical. Compared with tracheotomy, cricothyrotomy is quicker and easier to perform, does not require manipulation of the cervical spine, and is associated with fewer complications. However, while cricothyrotomy may be life-saving in extreme circumstances, this technique is only intended to be a temporizing measure until a definitive airway can be established.

The Combitube—also known as the esophageal tracheal airway or esophageal tracheal double-lumen airway—is a blind insertion airway device (BIAD) used in the pre-hospital and emergency setting. It is designed to provide an airway to facilitate the mechanical ventilation of a patient in respiratory distress.
Guedel's classification is a means of assessing the depth of general anesthesia introduced by Arthur Ernest Guedel (1883–1956) in 1920.
The following outline is provided as an overview of and topical guide to anesthesia:

The laryngeal tube is an airway management device designed as an alternative to other airway management techniques such as mask ventilation, laryngeal mask airway, and tracheal intubation. This device can be inserted blindly through the oropharynx into the hypopharynx to create an airway during anaesthesia and cardiopulmonary resuscitation so as to enable mechanical ventilation of the lungs.
Michael Frass is an Austrian medicine specialist for internal medicine and professor at the Medical University of Vienna (MUW). He is known for his work on homeopathy.

A blind insertion airway device is a medical device used for airway management that ensures an open pathway between a patient's lungs and the outside world, as well as reducing the risk of aspiration, which can be placed without visualization of the glottis. Blind insertion airway devices are often used in the pre-hospital and emergency setting.

Basic airway management is a concept and set of medical procedures performed to prevent and treat airway obstruction and allow for adequate ventilation to a patient's lungs. This is accomplished by clearing or preventing obstructions of airways. Airway obstructions can occur in both conscious and unconscious individuals. They can also be partial or complete. Airway obstruction is commonly caused by the tongue, the airways itself, foreign bodies or materials from the body itself, such as blood or vomit. Contrary to advanced airway management, basic airway management technique do not rely on the use of invasive medical equipment and can be performed with less training. Medical equipment commonly used includes oropharyngeal airway, nasopharyngeal airway, bag valve mask, and pocket mask. Airway management is a primary consideration in cardiopulmonary resuscitation, anaesthesia, emergency medicine, intensive care medicine and first aid.

Advanced airway management is the subset of airway management that involves advanced training, skill, and invasiveness. It encompasses various techniques performed to create an open or patent airway – a clear path between a patient's lungs and the outside world.

Intubation granuloma is a benign growth of granulation tissue in the larynx or trachea, which arises from tissue trauma due to endotracheal intubation. This medical condition is described as a common late complication of tracheal intubation, specifically caused by irritation to the mucosal tissue of the airway during insertion or removal of the patient's intubation tube.