The tibia, also known as the shinbone or shankbone, is the larger, stronger, and anterior (frontal) of the two bones in the leg below the knee in vertebrates, and it connects the knee with the ankle bones. The tibia is found on the medial side of the leg next to the fibula and closer to the median plane or centre-line. The tibia is connected to the fibula by the interosseous membrane of leg, forming a type of fibrous joint called a syndesmosis with very little movement. The tibia is named for the flute tibia. It is the second largest bone in the human body next to the femur. The leg bones are the strongest long bones as they support the rest of the body.
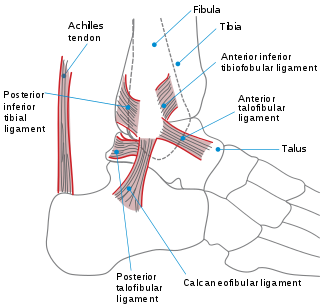
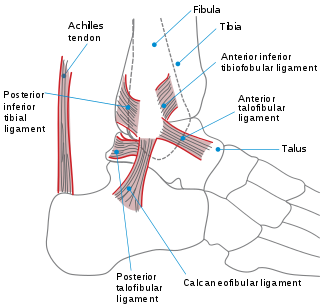
The ankle, or the talocrural region, or the jumping bone (informal) is the area where the foot and the leg meet. The ankle includes three joints: the ankle joint proper or talocrural joint, the subtalar joint, and the inferior tibiofibular joint. The movements produced at this joint are dorsiflexion and plantarflexion of the foot. In common usage, the term ankle refers exclusively to the ankle region. In medical terminology, "ankle" can refer broadly to the region or specifically to the talocrural joint.

Clearing the cervical spine is the process by which medical professionals determine whether cervical spine injuries exist, mainly regarding cervical fracture. It is generally performed in cases of major trauma. This process can take place in the emergency department or in the field by appropriately trained EMS personnel.

A bone fracture is a medical condition in which there is a partial or complete break in the continuity of a bone. In more severe cases, the bone may be broken into several pieces. A bone fracture may be the result of high force impact or stress, or a minimal trauma injury as a result of certain medical conditions that weaken the bones, such as osteoporosis, osteopenia, bone cancer, or osteogenesis imperfecta, where the fracture is then properly termed a pathologic fracture.

The Maisonneuve fracture is a spiral fracture of the proximal third of the fibula associated with a tear of the distal tibiofibular syndesmosis and the interosseous membrane. There is an associated fracture of the medial malleolus or rupture of the deep deltoid ligament of the ankle. This type of injury can be difficult to detect.

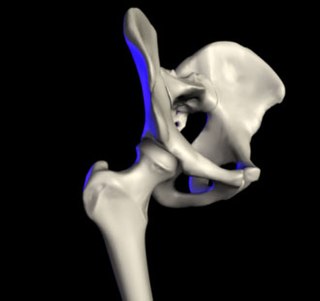
A joint dislocation, also called luxation, occurs when there is an abnormal separation in the joint, where two or more bones meet. A partial dislocation is referred to as a subluxation. Dislocations are often caused by sudden trauma on the joint like an impact or fall. A joint dislocation can cause damage to the surrounding ligaments, tendons, muscles, and nerves. Dislocations can occur in any joint major or minor. The most common joint dislocation is a shoulder dislocation.

A Lisfranc injury, also known as Lisfranc fracture, is an injury of the foot in which one or more of the metatarsal bones are displaced from the tarsus.

An ankle fracture is a break of one or more of the bones that make up the ankle joint. Symptoms may include pain, swelling, bruising, and an inability to walk on the injured leg. Complications may include an associated high ankle sprain, compartment syndrome, stiffness, malunion, and post-traumatic arthritis.
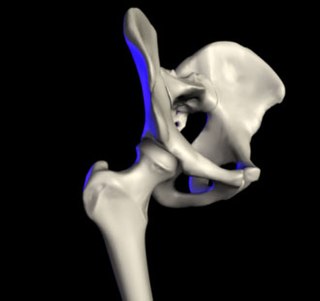
Transient synovitis of hip is a self-limiting condition in which there is an inflammation of the inner lining of the capsule of the hip joint. The term irritable hip refers to the syndrome of acute hip pain, joint stiffness, limp or non-weightbearing, indicative of an underlying condition such as transient synovitis or orthopedic infections. In everyday clinical practice however, irritable hip is commonly used as a synonym for transient synovitis. It should not be confused with sciatica, a condition describing hip and lower back pain much more common to adults than transient synovitis but with similar signs and symptoms.

A malleolus is the bony prominence on each side of the human ankle.

A calcaneal fracture is a break of the calcaneus. Symptoms may include pain, bruising, trouble walking, and deformity of the heel. It may be associated with breaks of the hip or back.

A trimalleolar fracture is a fracture of the ankle that involves the lateral malleolus, the medial malleolus, and the distal posterior aspect of the tibia, which can be termed the posterior malleolus. The trauma is sometimes accompanied by ligament damage and dislocation.

Recursive partitioning is a statistical method for multivariable analysis. Recursive partitioning creates a decision tree that strives to correctly classify members of the population by splitting it into sub-populations based on several dichotomous independent variables. The process is termed recursive because each sub-population may in turn be split an indefinite number of times until the splitting process terminates after a particular stopping criterion is reached.
A clinical prediction rule or clinical probability assessment specifies how to use medical signs, symptoms, and other findings to estimate the probability of a specific disease or clinical outcome.
A high ankle sprain, also known as a syndesmotic ankle sprain (SAS), is a sprain of the syndesmotic ligaments that connect the tibia and fibula in the lower leg, thereby creating a mortise and tenon joint for the ankle. High ankle sprains are described as high because they are located above the ankle. They comprise approximately 15% of all ankle sprains. Unlike the common lateral ankle sprains, when ligaments around the ankle are injured through an inward twisting, high ankle sprains are caused when the lower leg and foot externally rotates.
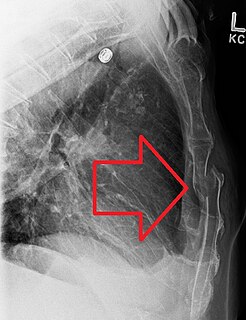
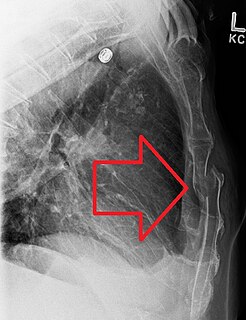
A sternal fracture is a fracture of the sternum, located in the center of the chest. The injury, which occurs in 5–8% of people who experience significant blunt chest trauma, may occur in vehicle accidents, when the still-moving chest strikes a steering wheel or dashboard or is injured by a seatbelt. Cardiopulmonary resuscitation (CPR), has also been known to cause thoracic injury, including sternum and rib fractures. Sternal fractures may also occur as a pathological fracture, in people who have weakened bone in their sternum, due to another disease process. Sternal fracture can interfere with breathing by making it more painful; however, its primary significance is that it can indicate the presence of serious associated internal injuries, especially to the heart and lungs.
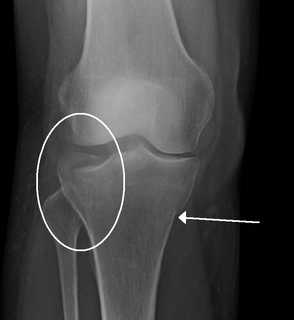
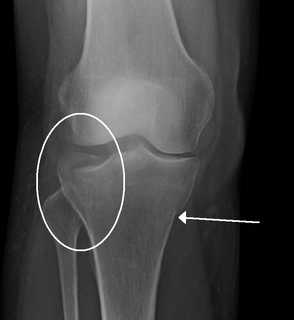
The Ottawa knee rules are a set of rules used to help physicians determine whether an x-ray of the knee is needed.
A crus fracture is a fracture of the lower legs bones meaning either or both of the tibia and fibula.
The Pittsburgh knee rules are medical rules created to ascertain whether a knee injury requires the use of X-ray to assess a fracture.
The Canadian CT head rule is a medical scale used to decide whether patients with minor head injuries should undergo cranial CT scans. It was originally described by Stiell et al. in a paper published in the Lancet in 2001, in which they initially used it only on patients with Glasgow Coma Scale scores of between 13 and 15. Since then, the CCTHR has become the most widely researched and extensively validated rule of its kind, though a 2011 systematic review noted that "its exclusion criteria make it difficult to apply universally."