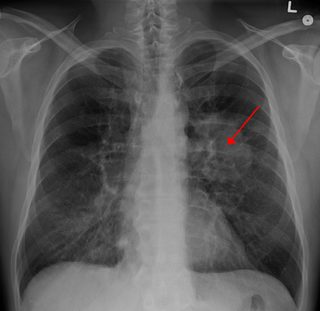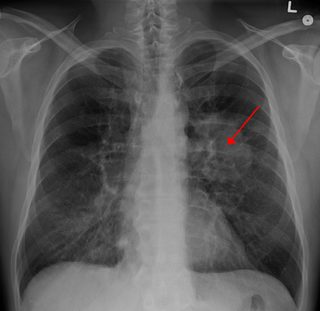
Lung cancer, also known as lung carcinoma, is a malignant tumor that begins in the lung. Lung cancer is caused by genetic damage to the DNA of cells in the airways, often caused by cigarette smoking or inhaling damaging chemicals. Damaged airway cells gain the ability to multiply unchecked, causing the growth of a tumor. Without treatment, tumors spread throughout the lung, damaging lung function. Eventually lung tumors metastasize, spreading to other parts of the body.

Ramsay Hunt syndrome type 2, commonly referred to simply as Ramsay Hunt syndrome (RHS) and also known as herpes zoster oticus, is inflammation of the geniculate ganglion of the facial nerve as a late consequence of varicella zoster virus (VZV). In regard to the frequency, less than 1% of varicella zoster infections involve the facial nerve and result in RHS. It is traditionally defined as a triad of ipsilateral facial paralysis, otalgia, and vesicles close to the ear and auditory canal. Due to its proximity to the vestibulocochlear nerve, the virus can spread and cause hearing loss, tinnitus, and vertigo. It is common for diagnoses to be overlooked or delayed, which can raise the likelihood of long-term consequences. It is more complicated than Bell's palsy. Therapy aims to shorten its overall length, while also providing pain relief and averting any consequences.

Sciatica is pain going down the leg from the lower back. This pain may go down the back, outside, or front of the leg. Onset is often sudden following activities like heavy lifting, though gradual onset may also occur. The pain is often described as shooting. Typically, symptoms are only on one side of the body. Certain causes, however, may result in pain on both sides. Lower back pain is sometimes present. Weakness or numbness may occur in various parts of the affected leg and foot.

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.
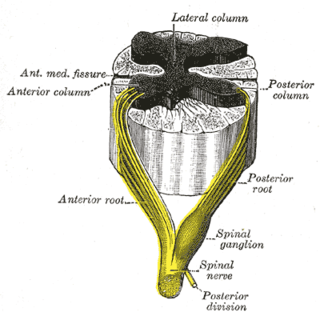
Spinal tumors are neoplasms located in either the vertebral column or the spinal cord. There are three main types of spinal tumors classified based on their location: extradural and intradural. Extradural tumors are located outside the dura mater lining and are most commonly metastatic. Intradural tumors are located inside the dura mater lining and are further subdivided into intramedullary and extramedullary tumors. Intradural-intramedullary tumors are located within the dura and spinal cord parenchyma, while intradural-extramedullary tumors are located within the dura but outside the spinal cord parenchyma. The most common presenting symptom of spinal tumors is nocturnal back pain. Other common symptoms include muscle weakness, sensory loss, and difficulty walking. Loss of bowel and bladder control may occur during the later stages of the disease.

Atelectasis is the partial collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct from pulmonary consolidation, in which they are filled with liquid. It is often referred to informally as a collapsed lung, although more accurately it usually involves only a partial collapse, and that ambiguous term is also informally used for a fully collapsed lung caused by a pneumothorax.

Horner's syndrome, also known as oculosympathetic paresis, is a combination of symptoms that arises when a group of nerves known as the sympathetic trunk is damaged. The signs and symptoms occur on the same side (ipsilateral) as it is a lesion of the sympathetic trunk. It is characterized by miosis, partial ptosis, apparent anhidrosis, with apparent enophthalmos.

The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve that supplies all the intrinsic muscles of the larynx, with the exception of the cricothyroid muscles. There are two recurrent laryngeal nerves, right and left. The right and left nerves are not symmetrical, with the left nerve looping under the aortic arch, and the right nerve looping under the right subclavian artery, then traveling upwards. They both travel alongside the trachea. Additionally, the nerves are among the few nerves that follow a recurrent course, moving in the opposite direction to the nerve they branch from, a fact from which they gain their name.

The stellate ganglion is a sympathetic ganglion formed by the fusion of the inferior cervical ganglion and the first thoracic ganglion, which is present in 80% of individuals. Sometimes, the second and the third thoracic ganglia are included in this fusion.

The pterygopalatine ganglion is a parasympathetic ganglion in the pterygopalatine fossa. It is one of four parasympathetic ganglia of the head and neck,.

A hamartoma is a mostly benign, local malformation of cells that resembles a neoplasm of local tissue but is usually due to an overgrowth of multiple aberrant cells, with a basis in a systemic genetic condition, rather than a growth descended from a single mutated cell (monoclonality), as would typically define a benign neoplasm/tumor. Despite this, many hamartomas are found to have clonal chromosomal aberrations that are acquired through somatic mutations, and on this basis the term hamartoma is sometimes considered synonymous with neoplasm. Hamartomas are by definition benign, slow-growing or self-limiting, though the underlying condition may still predispose the individual towards malignancies.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.
Meralgia paresthetica or meralgia paraesthetica is pain or abnormal sensations in the outer thigh not caused by injury to the thigh, but by injury to a nerve which provides sensation to the lateral thigh.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.

The lumbar ganglia are paravertebral ganglia located in the inferior portion of the sympathetic trunk. The lumbar portion of the sympathetic trunk typically has 4 lumbar ganglia. The lumbar splanchnic nerves arise from the ganglia here, and contribute sympathetic efferent fibers to the nearby plexuses. The first two lumbar ganglia have both white and gray rami communicates.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.

Adenocarcinoma of the lung is the most common type of lung cancer, and like other forms of lung cancer, it is characterized by distinct cellular and molecular features. It is classified as one of several non-small cell lung cancers (NSCLC), to distinguish it from small cell lung cancer which has a different behavior and prognosis. Lung adenocarcinoma is further classified into several subtypes and variants. The signs and symptoms of this specific type of lung cancer are similar to other forms of lung cancer, and patients most commonly complain of persistent cough and shortness of breath.
Interventional pain management or interventional pain medicine is a medical subspecialty defined by the National Uniforms Claims Committee (NUCC) as, " invasive interventions such as the discipline of medicine devoted to the diagnosis and treatment of pain related disorders principally with the application of interventional techniques in managing sub acute, chronic, persistent, and intractable pain, independently or in conjunction with other modalities of treatment". Medicare Payment Advisory Commission (MedPAC) defined interventional techniques as, "minimally invasive procedures including, percutaneous precision needle placement, with placement of drugs in targeted areas or ablation of targeted nerves; and some surgical techniques such as laser or endoscopic diskectomy, intrathecal infusion pumps and spinal cord stimulators, for the diagnosis and management of chronic, persistent or intractable pain". Minimally invasive interventions such as facet joint injections, nerve blocks, neuroaugmentation, vertebroplasty, kyphoplasty, nucleoplasty, endoscopic discectomy, and implantable drug delivery systems are utilized in managing subacute or chronic pain.
Cancer pain can be caused by pressure on, or chemical stimulation of, specialised pain-signalling nerve endings called nociceptors, or by damage or illness affecting nerve fibers themselves.
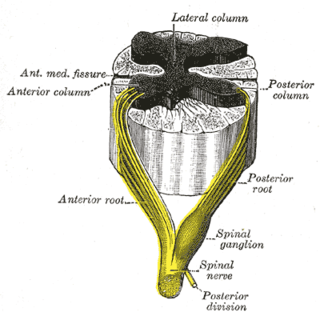
Sensory neuronopathy is a type of peripheral neuropathy that results primarily in sensory symptoms due to destruction of nerve cell bodies in the dorsal root ganglion. The causes of nerve damage are grouped into categories including those due to paraneoplastic causes, immune mediated, infectious, inherited or degenerative causes and those due to toxin exposure. In idiopathic sensory neuronopathy no cause is identified. Idiopathic causes account for about 50% of cases. Sensory neuronopathy differs from the more common length dependent axonal polyneuropathies in that the symptoms do not progress in a distal to proximal pattern, rather symptoms develop in a multifocal, asymmetric, and non-length dependent manner. Ataxia is a prominent symptom early in the disease course. The trigeminal nerve ganglion is also commonly affected leading to facial numbness. Motor nerves are usually not affected however some cases do have mild motor involvement in the form of weakness. Symptoms tend to develop sub-acutely, over weeks, in acquired sensory neuronopathy and more slowly in inherited or primary degenerative cases. In cases of paraneoplastic or infectious sensory neuropathy, treatment is directed at the underlying cancer or infectious cause respectively. Immunomodulatory and anti-inflammatory therapies are also commonly used however their effectiveness is limited.