Tubal ligation is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked, clipped or removed. This prevents the fertilization of eggs by sperm and thus the implantation of a fertilized egg. Tubal ligation is considered a permanent method of sterilization and birth control.

Hysterectomy is the surgical removal of the uterus. It may also involve removal of the cervix, ovaries (oophorectomy), Fallopian tubes (salpingectomy), and other surrounding structures.
Hemicorporectomy is a radical surgery in which the body below the waist is amputated, transecting the lumbar spine. This removes the legs, the genitalia, urinary system, pelvic bones, anus, and rectum. It is an extremely mutilating procedure recommended only as a last resort for people with severe and potentially fatal illnesses such as osteomyelitis, tumors, severe traumas and intractable decubiti in, or around, the pelvis. By 2009, 66 cases have been reported in medical literature. The most recent documented operation was in September 2019.

The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region below. Both males and females have a pelvic floor. To accommodate the birth canal, a female's pelvic cavity is larger than a male's.

A colostomy is an opening (stoma) in the large intestine (colon), or the surgical procedure that creates one. The opening is formed by drawing the healthy end of the colon through an incision in the anterior abdominal wall and suturing it into place. This opening, often in conjunction with an attached ostomy system, provides an alternative channel for feces to leave the body. Thus if the natural anus is unavailable for that function, an artificial anus takes over. It may be reversible or irreversible, depending on the circumstances.
In anatomy, a stoma is any opening in the body. For example, a mouth, a nose, and an anus are natural stomata. Any hollow organ can be manipulated into an artificial stoma as necessary. This includes the esophagus, stomach, duodenum, ileum, colon, pleural cavity, ureters, urinary bladder, and renal pelvis. Such a stoma may be permanent or temporary.
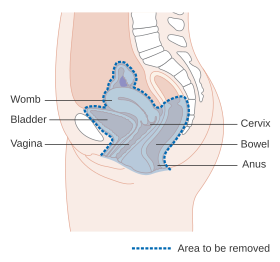
An abdomino perineal resection, formally known as abdominoperineal resection of the rectum and abdominoperineal excision of the rectum is a surgery for rectal cancer or anal cancer. It is frequently abbreviated as AP resection, APR and APER.

Pseudomyxoma peritonei (PMP) is a clinical condition caused by cancerous cells that produce abundant mucin or gelatinous ascites. The tumors cause fibrosis of tissues and impede digestion or organ function, and if left untreated, the tumors and mucin they produce will fill the abdominal cavity. This will result in compression of organs and will destroy the function of the colon, small intestine, stomach, or other organs. Prognosis with treatment in many cases is optimistic, but the disease is lethal if untreated, with death occurring via cachexia, bowel obstruction, or other types of complications.

Prostatectomy as a medical term refers to the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

Radical retropubic prostatectomy is a surgical procedure in which the prostate gland is removed through an incision in the abdomen. It is most often used to treat individuals who have early prostate cancer. Radical retropubic prostatectomy can be performed under general, spinal, or epidural anesthesia and requires blood transfusion less than one-fifth of the time. Radical retropubic prostatectomy is associated with complications such as urinary incontinence and impotence, but these outcomes are related to a combination of individual patient anatomy, surgical technique, and the experience and skill of the surgeon.

Vaginectomy is a surgery to remove all or part of the vagina. It is one form of treatment for individuals with vaginal cancer or rectal cancer that is used to remove tissue with cancerous cells. It can also be used in gender affirmation surgery. Some people born with a vagina who identify as transmasculine or as nonbinary may choose vaginectomy in conjunction with other surgeries to make the clitoris more penis-like (metoidioplasty), construct of a full-size penis (phalloplasty), or create a relatively smooth, featureless genital area.
Total mesorectal excision (TME) is a standard surgical technique for treatment of rectal cancer, first described in 1982 by Professor Bill Heald at the UK's Basingstoke District Hospital. It is a precise dissection of the mesorectal envelope comprising rectum containing the tumour together with all the surrounding fatty tissue and the sheet of tissue that contains lymph nodes and blood vessels. Dissection is along the avascular alveolar plane between the presacral and mesorectal fascia, described as holy plane. Dissection along this plane facilitates a straightforward dissection and preserves the sacral vessels and hypogastric nerves and is a sphincter-sparing resection and decreases permanent stoma rates. It is possible to rejoin the two ends of the colon; however, most patients require a temporary ileostomy pouch to bypass the colon, allowing it to heal with less risk of infection, perforation or leakage.
Coccygectomy is a surgical procedure in which the coccyx or tailbone is removed. It is considered a required treatment for sacrococcygeal teratoma and other germ cell tumors arising from the coccyx. Coccygectomy is the treatment of last resort for coccydynia which has failed to respond to nonsurgical treatment. Non surgical treatments include use of seat cushions, external or internal manipulation and massage of the coccyx and the attached muscles, medications given by local injections under fluoroscopic guidance, and medications by mouth.

A ureterostomy is the creation of a stoma for a ureter or kidney.

A pelvic examination is the physical examination of the external and internal female pelvic organs. It is frequently used in gynecology for the evaluation of symptoms affecting the female reproductive and urinary tract, such as pain, bleeding, discharge, urinary incontinence, or trauma. It can also be used to assess a woman's anatomy in preparation for procedures. The exam can be done awake in the clinic and emergency department, or under anesthesia in the operating room. The most commonly performed components of the exam are 1) the external exam, to evaluate the external genitalia 2) the internal exam with palpation to examine the uterus, ovaries, and fallopian tubes, and 3) the internal exam using the speculum to visualize the vaginal walls and cervix. During the pelvic exam, sample of cells and fluids may be collected to screen for sexually transmitted infections or cancer.

Urethrostomy is a surgical procedure that creates a permanent opening in the urethra, commonly to remove obstructions to urine flow. The procedure is most often performed in male cats, where the opening is made in the perineum.
Alexander Brunschwig was born in El Paso, Texas. He died in 1969 at the age of 67 of coronary disease.

The Wertheim–Meigs operation is a surgical procedure for the treatment of cervical cancer performed by way of an abdominal incision.

Prophylactic salpingectomy is a preventative surgical technique performed on patients who are at higher risk of having ovarian cancer, such as individuals who may have pathogenic variants of the BRCA1 or BRCA2 gene. Originally salpingectomy was used in cases of ectopic pregnancies. As a preventative surgery however, it involves the removal of the fallopian tubes. By not removing the ovaries this procedure is advantageous to individuals who are still of child bearing age. It also reduces risks such as cardiovascular disease and osteoporosis which are associated with removal of the ovaries.
Transvaginal mesh, also known as vaginal mesh implant, is a net-like surgical tool that is used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI) among female patients. The surgical mesh is placed transvaginally to reconstruct weakened pelvic muscle walls and to support the urethra or bladder.