Dilationand curettage (D&C) refers to the dilation of the cervix and surgical removal of sections and or layers of the lining of the uterus and or contents of the uterus such as an unwanted fetus, remains of a non viable fetus, retained placenta after birth or abortion as well as any abnormal tissue which may be in the uterus causing abnormal cycles by scraping and scooping (curettage). It is a gynecologic procedure used for treatment and removal as well as diagnostic and therapeutic purposes, and is the most commonly used method for first trimester abortion or miscarriage.

The uterus or womb is the organ in the reproductive system of most female mammals, including humans, that accommodates the embryonic and fetal development of one or more embryos until birth. The uterus is a hormone-responsive sex organ that contains glands in its lining that secrete uterine milk for embryonic nourishment.

Asherman's syndrome (AS) is an acquired uterine condition that occurs when scar tissue (adhesions) forms inside the uterus and/or the cervix. It is characterized by variable scarring inside the uterine cavity, where in many cases the front and back walls of the uterus stick to one another. AS can be the cause of menstrual disturbances, infertility, and placental abnormalities. Although the first case of intrauterine adhesion was published in 1894 by Heinrich Fritsch, it was only after 54 years that a full description of Asherman syndrome was carried out by Joseph Asherman. A number of other terms have been used to describe the condition and related conditions including: uterine/cervical atresia, traumatic uterine atrophy, sclerotic endometrium, and endometrial sclerosis.

Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus (endometrium) atypically located among the cells of the uterine wall (myometrium), as a result, thickening of the uterus occurs. As well as being misplaced in patients with this condition, endometrial tissue is completely functional. The tissue thickens, sheds and bleeds during every menstrual cycle.

Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reproductive system, such as abnormal uterine bleeding.

Falloposcopy is the inspection of the fallopian tubes through a micro- endoscope. The falloposcope is inserted into the tube through its opening in the uterus at the proximal tubal opening via the uterotubal junction; technically it could also be inserted at the time of abdominal surgery or laparoscopy via the distal fimbriated end.

Gynecologic ultrasonography or gynecologic sonography refers to the application of medical ultrasonography to the female pelvic organs as well as the bladder, the adnexa, and the recto-uterine pouch. The procedure may lead to other medically relevant findings in the pelvis.This technique is useful to detect myomas or mullerian malformations.
Cervical dilation is the opening of the cervix, the entrance to the uterus, during childbirth, miscarriage, induced abortion, or gynecological surgery. Cervical dilation may occur naturally, or may be induced surgically or medically.

A uterine malformation is a type of female genital malformation resulting from an abnormal development of the Müllerian duct(s) during embryogenesis. Symptoms range from amenorrhea, infertility, recurrent pregnancy loss, and pain, to normal functioning depending on the nature of the defect.

An endometrial polyp or uterine polyp is a mass in the inner lining of the uterus. They may have a large flat base (sessile) or be attached to the uterus by an elongated pedicle (pedunculated). Pedunculated polyps are more common than sessile ones. They range in size from a few millimeters to several centimeters. If pedunculated, they can protrude through the cervix into the vagina. Small blood vessels may be present, particularly in large polyps.

Myomectomy, sometimes also called fibroidectomy, refers to the surgical removal of uterine leiomyomas, also known as fibroids. In contrast to a hysterectomy, the uterus remains preserved and the woman retains her reproductive potential. It still may impact hormonal regulation and the menstrual cycle.

Vacuum or suction aspiration is a procedure that uses a vacuum source to remove an embryo or fetus through the cervix. The procedure is performed to induce abortion, as a treatment for incomplete spontaneous abortion or retained fetal and placental tissue, or to obtain a sample of uterine lining. It is generally safe, and serious complications rarely occur.
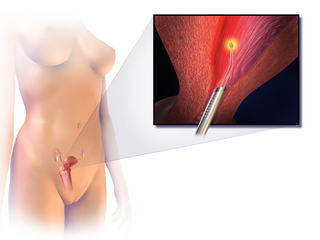
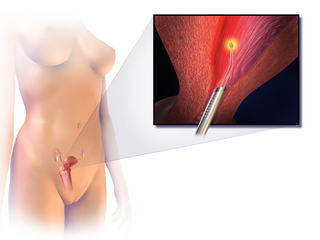
Endometrial ablation is a surgical procedure that is used to remove (ablate) or destroy the endometrial lining of the uterus. The goal of the procedure is to decrease the amount of blood loss during menstrual periods. Endometrial ablation is most often employed in people with excessive menstrual bleeding, who do not wish to undergo a hysterectomy, following unsuccessful medical therapy.

A unicornuate uterus represents a uterine malformation where the uterus is formed from one only of the paired Müllerian ducts while the other Müllerian duct does not develop or only in a rudimentary fashion. The sometimes called hemi-uterus has a single horn linked to the ipsilateral fallopian tube that faces its ovary.

The arcuate uterus is a form of a uterine anomaly or variation where the uterine cavity displays a concave contour towards the fundus. Normally the uterine cavity is straight or convex towards the fundus on anterior-posterior imaging, but in the arcuate uterus the myometrium of the fundus dips into the cavity and may form a small septation. The distinction between an arcuate uterus and a septate uterus is not standardized.
A uterine septum is a congenital uterine malformation where the uterine cavity is partitioned by a longitudinal septum; the outside of the uterus has a normal typical shape. The wedge-like partition may involve only the superior part of the cavity resulting in an incomplete septum or a subseptate uterus, or less frequently the total length of the cavity and the cervix resulting in a double cervix. The septation may also continue caudally into the vagina resulting in a "double vagina".
Tubal reversal, also called tubal sterilization reversal, tubal ligation reversal, or microsurgical tubal reanastomosis, is a surgical procedure that can restore fertility to women after a tubal ligation. By rejoining the separated segments of the fallopian tube, tubal reversal can give women the chance to become pregnant again. In some cases, however, the separated segments cannot actually be reattached to each other. In some cases the remaining segment of tube needs to be re-implanted into the uterus. In other cases, when the end of the tube has been removed, a procedure called a neofimbrioplasty must be performed to recreate a functional end of the tube which can then act like the missing fimbria and retrieve the egg that has been released during ovulation.

Hematometra is a medical condition involving collection or retention of blood in the uterus. It is most commonly caused by an imperforate hymen or a transverse vaginal septum.

Osmotic dilators are medical implements used to dilate the uterine cervix by swelling as they absorb fluid from surrounding tissue. They may be composed of natural or synthetic materials. A laminaria stick or tent is a thin rod made of the stems of dried Laminaria, a genus of kelp. Laminaria sticks can be generated from Laminaria japonica and Laminaria digitata. Synthetic osmotic dilators are commonly referred to by their brand names, such as Dilapan. Dilapan-S are composed of polyacrylonitrile, a plastic polymer. The hygroscopic nature of the polymer causes the dilator to absorb fluid and expand.

Hysterosalpingography (HSG), also known as uterosalpingography, is a radiologic procedure to investigate the shape of the uterine cavity and the shape and patency of the fallopian tubes. It is a special x-ray procedure using dye to look at the womb (uterus) and fallopian tubes. In this procedure, a radio-opaque material is injected into the cervical canal, and radiographs are taken. A normal result shows the filling of the uterine cavity and the bilateral filling of the fallopian tube with the injection material. To demonstrate tubal patency, spillage of the material into the peritoneal cavity needs to be observed. Hysterosalpingography has vital role in treatment of infertility, especially in the case of fallopian tube blockage.