An endoscopy is a procedure used in medicine to look inside the body. The endoscopy procedure uses an endoscope to examine the interior of a hollow organ or cavity of the body. Unlike many other medical imaging techniques, endoscopes are inserted directly into the organ.

A speculum is a medical tool for investigating body orifices, with a form dependent on the orifice for which it is designed. In old texts, the speculum may also be referred to as a diopter or dioptra. Like an endoscope, a speculum allows a view inside the body; endoscopes, however, tend to have optics while a speculum is intended for direct vision.

Colonoscopy or coloscopy is a medical procedure involving the endoscopic examination of the large bowel (colon) and the distal portion of the small bowel. This examination is performed using either a CCD camera or a fiber optic camera, which is mounted on a flexible tube and passed through the anus.
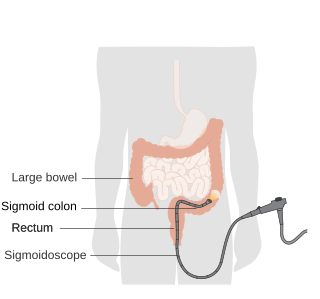
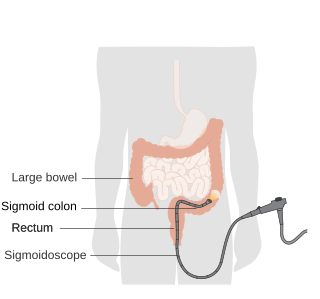
Sigmoidoscopy is the minimally invasive medical examination of the large intestine from the rectum through to the nearest part of the colon, the sigmoid colon. There are two types of sigmoidoscopy: flexible sigmoidoscopy, which uses a flexible endoscope, and rigid sigmoidoscopy, which uses a rigid device. Flexible sigmoidoscopy is generally the preferred procedure. A sigmoidoscopy is similar to, but not the same as, a colonoscopy. A sigmoidoscopy only examines up to the sigmoid, the most distal part of the colon, while colonoscopy examines the whole large bowel.
An endoscope is an inspection instrument composed of image sensor, optical lens, light source and mechanical device, which is used to look deep into the body by way of openings such as the mouth or anus. A typical endoscope applies several modern technologies including optics, ergonomics, precision mechanics, electronics, and software engineering. With an endoscope, it is possible to observe lesions that cannot be detected by X-ray, making it useful in medical diagnosis. An endoscope uses tubes only a few millimeters thick to transfer illumination in one direction and high-resolution video in the other, allowing minimally invasive surgeries. It is used to examine the internal organs like the throat or esophagus. Specialized instruments are named after their target organ. Examples include the cystoscope (bladder), nephroscope (kidney), bronchoscope (bronchus), arthroscope (joints) and colonoscope (colon), and laparoscope. They can be used to examine visually and diagnose, or assist in surgery such as an arthroscopy.
Rubber band ligation (RBL) is an outpatient treatment procedure for internal hemorrhoids of any grade. There are several different devices a physician may use to perform the procedure, including the traditional metal devices, endoscopic banding, and the CRH O'Regan System.

A rectal prolapse occurs when walls of the rectum have prolapsed to such a degree that they protrude out of the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on whether the prolapsed section is visible externally, and whether the full or only partial thickness of the rectal wall is involved.

Rectal foreign bodies are large foreign items found in the rectum that can be assumed to have been inserted through the anus, rather than reaching the rectum via the mouth and gastrointestinal tract. It can be of clinical relevance if the patient cannot remove it the way they intended. Smaller, ingested foreign bodies, such as bones eaten with food, can sometimes be found stuck in the rectum upon X-ray and are rarely of clinical relevance.

Colorectal surgery is a field in medicine dealing with disorders of the rectum, anus, and colon. The field is also known as proctology, but this term is now used infrequently within medicine and is most often employed to identify practices relating to the anus and rectum in particular. The word proctology is derived from the Greek words πρωκτός proktos, meaning "anus" or "hindparts", and -λογία -logia, meaning "science" or "study".
Rectal bleeding refers to bleeding in the rectum, thus a form of lower gastrointestinal bleeding. There are many causes of rectal hemorrhage, including inflamed hemorrhoids, rectal varices, proctitis, stercoral ulcers, and infections. Diagnosis is usually made by proctoscopy, which is an endoscopic test.

Anal fistula is a chronic abnormal communication between the anal canal and the perianal skin. An anal fistula can be described as a narrow tunnel with its internal opening in the anal canal and its external opening in the skin near the anus. Anal fistulae commonly occur in people with a history of anal abscesses. They can form when anal abscesses do not heal properly.

Endoscopic ultrasound (EUS) or echo-endoscopy is a medical procedure in which endoscopy is combined with ultrasound to obtain images of the internal organs in the chest, abdomen and colon. It can be used to visualize the walls of these organs, or to look at adjacent structures. Combined with Doppler imaging, nearby blood vessels can also be evaluated.

An anoscopy is a medical examination using a small, rigid, tubular instrument called an anoscope. This is inserted a few inches into the anus in order to evaluate problems of the anal canal. Anoscopy is used to diagnose hemorrhoids, anal fissures, and some cancers.

The middle rectal artery is an artery in the pelvis that supplies blood to the rectum.

An anal plug is a medical device that is often used to treat fecal incontinence, the accidental passing of bowel moments, by physically blocking involuntary loss of fecal material. Fecal material such as feces are solid remains of food that does not get digested in the small intestines; rather, it is broken down by bacteria in the large intestine. Anal plugs vary in design and composition, but they are typically single-use, intra-anal, disposable devices made out of soft materials to contain fecal material and prevent it from leaking out of the rectum. The idea of an anal insert for fecal incontinence was first evaluated in a study of 10 participants with three different designs of anal inserts.

A pelvic examination is the physical examination of the external and internal female pelvic organs. It is frequently used in gynecology for the evaluation of symptoms affecting the female reproductive and urinary tract, such as pain, bleeding, discharge, urinary incontinence, or trauma. It can also be used to assess a woman's anatomy in preparation for procedures. The exam can be done awake in the clinic and emergency department, or under anesthesia in the operating room. The most commonly performed components of the exam are 1) the external exam, to evaluate the vulva 2) the internal exam with palpation to examine the uterus, ovaries, and structures adjacent to the uterus (adnexae) and 3) the internal exam using a speculum to visualize the vaginal walls and cervix. During the pelvic exam, sample of cells and fluids may be collected to screen for sexually transmitted infections or cancer.

The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about 12 centimetres (4.7 in) long, and begins at the rectosigmoid junction at the level of the third sacral vertebra or the sacral promontory depending upon what definition is used. Its diameter is similar to that of the sigmoid colon at its commencement, but it is dilated near its termination, forming the rectal ampulla. It terminates at the level of the anorectal ring or the dentate line, again depending upon which definition is used. In humans, the rectum is followed by the anal canal, which is about 4 centimetres (1.6 in) long, before the gastrointestinal tract terminates at the anal verge. The word rectum comes from the Latin rēctumintestīnum, meaning straight intestine.
Solitary rectal ulcer syndrome or SRUS is a chronic disorder of the rectal mucosa. It commonly occurs with varying degrees of rectal prolapse. The condition is thought to be caused by different factors, such as long term constipation, straining during defecation, and dyssynergic defecation. Treatment is by normalization of bowel habits, biofeedback, and other conservative measures. In more severe cases various surgical procedures may be indicated. The condition is relatively rare, affecting approximately 1 in 100,000 people per year. It affects mainly adults aged 30–50. Females are affected slightly more often than males. The disorder can be confused clinically with rectal cancer or other conditions such as inflammatory bowel disease, even when a biopsy is done.
Obstructed defecation syndrome is a major cause of functional constipation, of which it is considered a subtype. It is characterized by difficult and/or incomplete emptying of the rectum with or without an actual reduction in the number of bowel movements per week. Normal definitions of functional constipation include infrequent bowel movements and hard stools. In contrast, ODS may occur with frequent bowel movements and even with soft stools, and the colonic transit time may be normal, but delayed in the rectum and sigmoid colon.

A rectal or anal dilator is a medical device similar to a speculum designed to open and relax the internal/external anal sphincter and rectum in order to facilitate medical inspection or relieve constipation. One early version of a rectal dilator was Dr. Young's Ideal Rectal Dilators, invented in 1892.