Related Research Articles

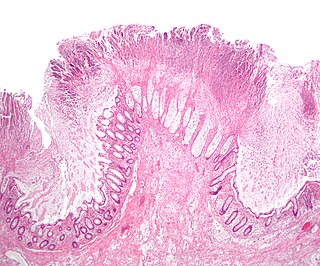
Crohn's disease is a type of inflammatory bowel disease (IBD) that may affect any segment of the gastrointestinal tract. Symptoms often include abdominal pain, diarrhea, fever, abdominal distension, and weight loss. Complications outside of the gastrointestinal tract may include anemia, skin rashes, arthritis, inflammation of the eye, and fatigue. The skin rashes may be due to infections as well as pyoderma gangrenosum or erythema nodosum. Bowel obstruction may occur as a complication of chronic inflammation, and those with the disease are at greater risk of colon cancer and small bowel cancer.

Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs and symptoms include abdominal pain, vomiting, bloating and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital.

Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, with Crohn's disease and ulcerative colitis (UC) being the principal types. Crohn's disease affects the small intestine and large intestine, as well as the mouth, esophagus, stomach and the anus, whereas UC primarily affects the colon and the rectum.

Short bowel syndrome is a rare malabsorption disorder caused by a lack of functional small intestine. The primary symptom is diarrhea, which can result in dehydration, malnutrition, and weight loss. Other symptoms may include bloating, heartburn, feeling tired, lactose intolerance, and foul-smelling stool. Complications can include anemia and kidney stones.

Ileostomy is a stoma constructed by bringing the end or loop of small intestine out onto the surface of the skin, or the surgical procedure which creates this opening. Intestinal waste passes out of the ileostomy and is collected in an external ostomy system which is placed next to the opening. Ileostomies are usually sited above the groin on the right hand side of the abdomen.

A volvulus is when a loop of intestine twists around itself and the mesentery that supports it, resulting in a bowel obstruction. Symptoms include abdominal pain, abdominal bloating, vomiting, constipation, and bloody stool. Onset of symptoms may be rapid or more gradual. The mesentery may become so tightly twisted that blood flow to part of the intestine is cut off, resulting in ischemic bowel. In this situation there may be fever or significant pain when the abdomen is touched.
Colectomy is bowel resection of the large bowel. It consists of the surgical removal of any extent of the colon, usually segmental resection. In extreme cases where the entire large intestine is removed, it is called total colectomy, and proctocolectomy denotes that the rectum is included.
Proctitis is an inflammation of the anus and the lining of the rectum, affecting only the last 6 inches of the rectum.

Anal fistula is a chronic abnormal communication between the anal canal and the perianal skin. An anal fistula can be described as a narrow tunnel with its internal opening in the anal canal and its external opening in the skin near the anus. Anal fistulae commonly occur in people with a history of anal abscesses. They can form when anal abscesses do not heal properly.

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply. Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.

A bowel resection or enterectomy is a surgical procedure in which a part of an intestine (bowel) is removed, from either the small intestine or large intestine. Often the word enterectomy is reserved for the sense of small bowel resection, in distinction from colectomy, which covers the sense of large bowel resection. Bowel resection may be performed to treat gastrointestinal cancer, bowel ischemia, necrosis, or obstruction due to scar tissue, volvulus, and hernias. Some patients require ileostomy or colostomy after this procedure as alternative means of excretion. Complications of the procedure may include anastomotic leak or dehiscence, hernias, or adhesions causing partial or complete bowel obstruction. Depending on which part and how much of the intestines are removed, there may be digestive and metabolic challenges afterward, such as short bowel syndrome.
Jejunoileal bypass (JIB) was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel were detached and set to the side.
Intestinal Connective tissue abnormality may cause Intestinal Desmosis The absence of the tendinous plexus layer was first described in 1998 by Meier-Ruge. Desmosis is implicated in disturbed gut motility.
Serial transverse enteroplasty (STEP) is a surgical procedure used primarily in the treatment of short bowel syndrome (SBS). In STEP, by making cuts in the intestine and creating a zigzag pattern, surgeons lengthen the amount of bowel available to absorb nutrients. The procedure was first performed in 2003 and more than 100 patients had undergone the surgery by 2013.

Intestine transplantation is the surgical replacement of the small intestine for chronic and acute cases of intestinal failure. While intestinal failure can oftentimes be treated with alternative therapies such as parenteral nutrition (PN), complications such as PN-associated liver disease and short bowel syndrome may make transplantation the only viable option. One of the rarest type of organ transplantation performed, intestine transplantation is becoming increasingly prevalent as a therapeutic option due to improvements in immunosuppressive regimens, surgical technique, PN, and the clinical management of pre and post-transplant patients.
Heineke–Mikulicz Strictureplasty is the most common among the conventional strictureplasties. Emmanuel Lee introduced this strictureplasty for the treatment of Crohn's disease in 1976. A similar technique for tubercular strictures of the terminal ileum was reported by RN Katariya et al. in 1977 This technique is similar to a Heineke–Mikulicz pyloroplasty from which it derives its name.
Finney strictureplasty is indicated for strictures up to 15 centimeters. The Finney strictureplasty is performed by folding the diseased bowel on itself and creating a large opening between the two loops. This strictureplasty can be used to address longer strictures than those manageable with the Heineke-Mikulicz technique.
The side-to-side isoperistaltic strictureplasty, also now known as the Michelassi stricureplasty, was designed to avoid sacrificing large amounts of small bowel in case of long segments of stricturing Crohn's disease.
Fabrizio Michelassi, M.D., F.A.C.S. is the Lewis Atterbury Stimson Professor, and Chairman of the Department of Surgery at Weill Cornell Medicine and Surgeon-in-Chief at NewYork-Presbyterian/Weill Cornell Medical Center.

Choledochoduodenostomy (CDD) is a surgical procedure to create an anastomosis, a surgical connection, between the common bile duct (CBD) and an alternative portion of the duodenum. In healthy individuals, the CBD meets the pancreatic duct at the ampulla of Vater, which drains via the major duodenal papilla to the second part of duodenum. In cases of benign conditions such as narrowing of the distal CBD or recurrent CBD stones, performing a CDD provides the diseased patient with CBD drainage and decompression. A side-to-side anastomosis is usually performed.
References
- ↑ Lee EC, Papaioannou N (July 1982). "Minimal surgery for chronic obstruction in patients with extensive or universal Crohn's disease". Ann R Coll Surg Engl. 64 (4): 229–33. PMC 2494172 . PMID 7092090.
- ↑ Hurst RD, Michelassi F (April 1998). "Strictureplasty for Crohn's disease: techniques and long-term results". World J Surg. 22 (4): 359–63. doi:10.1007/s002689900397. PMID 9523517. S2CID 31003228.
- ↑ Michelassi F (March 1996). "Side-to-side isoperistaltic strictureplasty for multiple Crohn's strictures". Dis. Colon Rectum. 39 (3): 345–9. doi:10.1007/bf02049480. PMID 8603560. S2CID 42067049.
- ↑ Fazio VW, et al. (1989). "Strictureplasty in Crohn's Disease". Ann. Surg. 210 (5): 621–625. doi:10.1097/00000658-198911000-00009. PMC 1357796 . PMID 2818031.
- ↑ Rigazio C, Ercole E, Maconi G (2013-09-21). Giovanni Maconi, Gabriele Bianchi Porro (ed.). Ultrasound of the Gastrointestinal Tract. Springer Science & Business Media. pp. 7–17. ISBN 978-3-642-31983-9.