Gastric bypass surgery refers to a technique in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass procedures (GBP). Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.
A gastrectomy is a partial or total surgical removal of the stomach.
Bypass surgery refers to a class of surgery involving rerouting a tubular body part.
The duodenal switch (DS) procedure, gastric reduction duodenal switch (GRDS), is a weight loss surgery procedure that is composed of a restrictive and a malabsorptive aspect.

A laparoscopic adjustable gastric band, commonly called a lap-band, A band, or LAGB, is an inflatable silicone device placed around the top portion of the stomach to treat obesity, intended to decrease food consumption.

Sleeve gastrectomy or vertical sleeve gastrectomy, is a surgical weight-loss procedure, typically performed laparoscopically, in which approximately 75 - 85% of the stomach is removed, along the greater curvature, which leaves a cylindrical, or "sleeve"-shaped stomach the size of a banana. Weight loss is affected not only through the reduction of the organ's size, but by the removal of the portion of it that produces ghrelin, the hormone that stimulates appetite. Patients can lose 50-70 percent of excess weight over the course of the two years that follow the surgery. The procedure is irreversible, though in some uncommon cases, patients can regain the lost weight, via resumption of poor dietary habits, or dilation of the stomach over time, which can require gastric sleeve revision surgery to either repair the sleeve or convert it to another type of weight loss method that may produce better results, such as a gastric bypass or duodenal switch.
Bariatric surgery is a medical term for surgical procedures used to manage obesity and obesity-related conditions. Long term weight loss with bariatric surgery may be achieved through alteration of gut hormones, physical reduction of stomach size, reduction of nutrient absorption, or a combination of these. Standard of care procedures include Roux en-Y bypass, sleeve gastrectomy, and biliopancreatic diversion with duodenal switch, from which weight loss is largely achieved by altering gut hormone levels responsible for hunger and satiety, leading to a new hormonal weight set point.
StomaphyX is an endoscopic suturing system designed to treat patients who have had previous Roux-en-Y gastric bypass surgery. Following this surgery, the stomach pouch and stomach outlet (stoma) becomes enlarged in some patients. The StomaphyX device can be used to restrict the size of the stoma without exposing the patient to further surgical risk.
Jejunoileal bypass (JIB) was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel were detached and set to the side.
Revision weight loss surgery is a surgical procedure that is performed on patients who have already undergone a form of bariatric surgery, and have either had complications from such surgery or have not achieved significant weight loss results from the initial surgery. Procedures are usually performed laparoscopically, though open surgery may be required if prior bariatric surgery has resulted in extensive scarring.
Lubomyr Kuzmak was a pioneer within the bariatric surgical community inventing the adjustable silicone band.

Gastric electrical stimulation, also known as implantable gastric stimulation, is the use of specific devices to provide electrical stimulation to the stomach to try to bring about weight loss in those who are overweight or improve gastroparesis.

SADI-S is a bariatric surgical technique to address metabolic disorders and to lose weight. It is a variation on the Duodenal Switch surgery, incorporating a vertical sleeve gastrectomy with a gastric bypass technique.
A duodenal-jejunal bypass liner, commonly called an EndoBarrier, is an implantable medical device in the form of a thin flexible 60 cm-long tube that creates a physical barrier between ingested food and the duodenum/proximal jejunum. The duodenal-jejunal bypass liner prevents the interaction of food with enzymes and hormones in the proximal intestine to treat type 2 diabetes and obesity. The duodenal-jejunal bypass liner is delivered endoscopically and has been tested on the morbidly obese as well as obese patients with a BMI less than 40, particularly those with difficult-to-manage type 2 diabetes. Despite a handful of serious adverse events such as gastrointestinal bleeding, abdominal pain, and device migration — all resolved with device removal — initial clinical trials have produced promising results in the treatment's ability to improve weight loss and glucose homeostasis outcomes.
Aspiration therapy is a bariatric approach to siphon ingested food from the stomach via an implanted tube and port to the outside of the body to be discarded. The device for this approach was developed by researchers at Washington University in St. Louis to treat obesity and has been named AspireAssist. The device has also been termed a reverse feeding tube. It was approved by the Food and Drug Administration (FDA) on June 14, 2016.
Stomach Intestinal Pylorus-Sparing (SIPS) surgery is a type of weight-loss surgery. It was developed in 2013 by two U.S. surgeons, Daniel Cottam from Utah and Mitchell S. Roslin from New York.
In medicine, endoscopic sleeve gastroplasty (ESG) is a minimally-invasive, non-surgical (incisionless), endoscopic weight loss procedure that is part of the field of endoscopic bariatric therapies. To perform ESG, a physician sutures a patient’s stomach into a narrower, smaller tube-like configuration. The result is a more restricted stomach that forces patients to feel fuller sooner, eating fewer calories, which facilitates weight loss.
Intestinal bypass is a bariatric surgery performed on patients with morbid obesity to create an irreversible weight loss, when implementing harsh restrictions on the diets have failed. Jejunocolic anastomosis was firstly employed. Nonetheless, it led to some unexpected complications such as severe electrolyte imbalance and liver failure. It was then modified to jejunoileal techniques. Viewed as a novel form of treatment for obesity, many intestinal bypass operations were carried out in the 1960s and 1980s. Significant weight loss was observed in patients, but this surgery also resulted in several complications, for instance, nutritional deficiencies and metabolic problems. Due to the presence of surgical alternatives and anti-obesity medications, intestinal bypass is now rarely used.
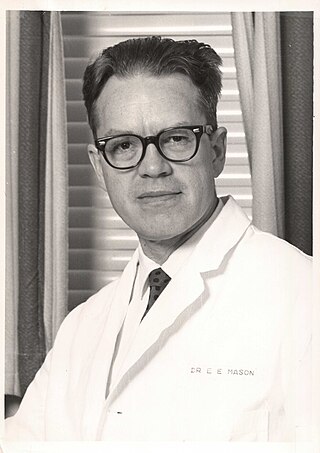
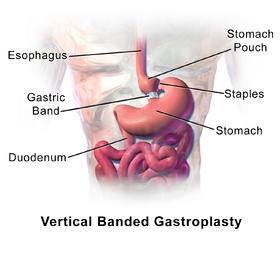
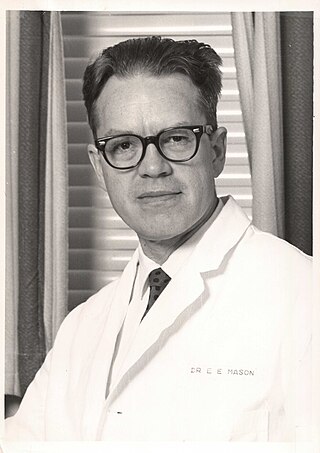
Edward Eaton Mason was an American surgeon, professor, and medical researcher who specialized in obesity surgery. He is known for developing restrictive gastric surgery for morbidly obese patients. Mason introduced the first gastric bypass surgery in 1966 and was the inventor of the first vertical banded gastroplasty surgery in 1980.

Antrectomy, also called distal gastrectomy, is a type of gastric resection surgery that involves the removal of the stomach antrum to treat gastric diseases causing the damage, bleeding, or blockage of the stomach. This is performed using either the Billroth I (BI) or Billroth II (BII) reconstruction method. Quite often, antrectomy is used alongside vagotomy to maximise its safety and effectiveness. Modern antrectomies typically have a high success rate and low mortality rate, but the exact numbers depend on the specific conditions being treated.