Related Research Articles

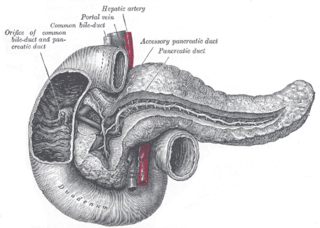
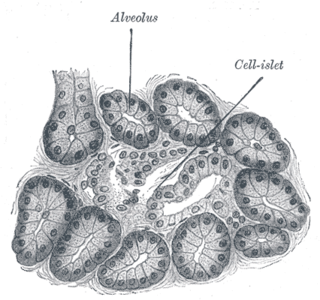
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types: acute pancreatitis, and chronic pancreatitis.

Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of pancreatic cancer are known.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes include a gallstone impacted in the common bile duct or the pancreatic duct, heavy alcohol use, systemic disease, trauma, elevated calcium levels, hypertriglyceridemia, certain medications, hereditary causes and, in children, mumps. Acute pancreatitis may be a single event, it may be recurrent, or it may progress to chronic pancreatitis and/or pancreatic failure.

Chronic pancreatitis is a long-standing inflammation of the pancreas that alters the organ's normal structure and functions. It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. It is a disease process characterized by irreversible damage to the pancreas as distinct from reversible changes in acute pancreatitis. Tobacco smoke and alcohol misuse are two of the most frequently implicated causes, and the two risk factors are thought to have a synergistic effect with regards to the development of chronic pancreatitis. Chronic pancreatitis is a risk factor for the development of pancreatic cancer.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.
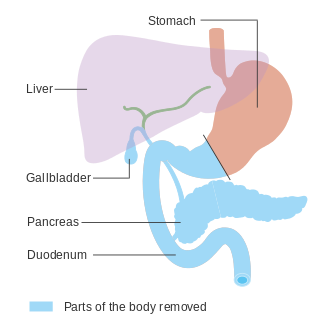
In medicine, a pancreatectomy is the surgical removal of all or part of the pancreas. Several types of pancreatectomy exist, including pancreaticoduodenectomy, distal pancreatectomy, segmental pancreatectomy, and total pancreatectomy. In total pancreatectomy, the gallbladder, distal stomach, a portion of the small intestine, associated lymph nodes and in certain cases the spleen are removed in addition to the entire pancreas. In recent years, the TP-IAT has also gained respectable traction within the medical community. These procedures are used in the management of several conditions involving the pancreas, such as benign pancreatic tumors, pancreatic cancer, and pancreatitis.

A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

Pseudocysts are like cysts, but lack epithelial or endothelial cells. Initial management consists of general supportive care. Symptoms and complications caused by pseudocysts require surgery. Computed tomography (CT) scans are used for initial imaging of cysts, and endoscopic ultrasounds are used in differentiating between cysts and pseudocysts. Endoscopic drainage is a popular and effective method of treating pseudocysts.

A pancreatic fistula is an abnormal communication between the pancreas and other organs due to leakage of pancreatic secretions from damaged pancreatic ducts. An external pancreatic fistula is one that communicates with the skin, and is also known as a pancreaticocutaneous fistula, whereas an internal pancreatic fistula communicates with other internal organs or spaces. Pancreatic fistulas can be caused by pancreatic disease, trauma, or surgery.

Pancreas divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts. Most individuals with pancreas divisum remain without symptoms or complications. A minority of people with pancreatic divisum may develop episodes of abdominal pain, nausea or vomiting due to acute or chronic pancreatitis. The presence of pancreas divisum is usually identified with cross sectional diagnostic imaging, such as endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP). In some cases, it may be detected intraoperatively. If no symptoms or complications are present, then treatment is not necessary. However, if there is recurrent pancreatitis, then a sphincterotomy of the minor papilla may be indicated.
Pancreatic diseases are diseases that affect the pancreas, an organ in most vertebrates and in humans and other mammals located in the abdomen. The pancreas plays a role in the digestive and endocrine system, producing enzymes which aid the digestion process and the hormone insulin, which regulates blood sugar levels. The most common pancreatic disease is pancreatitis, an inflammation of the pancreas which could come in acute or chronic form. Other pancreatic diseases include diabetes mellitus, exocrine pancreatic insufficiency, cystic fibrosis, pseudocysts, cysts, congenital malformations, tumors including pancreatic cancer, and hemosuccus pancreaticus.

Hemosuccus pancreaticus is a rare cause of hemorrhage in the gastrointestinal tract. It is caused by a bleeding source in the pancreas, pancreatic duct, or structures adjacent to the pancreas, such as the splenic artery, that bleed into the pancreatic duct, which is connected with the bowel at the duodenum, the first part of the small intestine. Patients with hemosuccus may develop symptoms of gastrointestinal hemorrhage, such as blood in the stools, maroon stools, or melena, which is a dark, tarry stool caused by digestion of red blood cells. They may also develop abdominal pain. It is associated with pancreatitis, pancreatic cancer and aneurysms of the splenic artery. Hemosuccus may be identified with endoscopy (esophagogastroduodenoscopy), where fresh blood may be seen from the pancreatic duct. Alternatively, angiography may be used to inject the celiac axis to determine the blood vessel that is bleeding. This may also be used to treat hemosuccus, as embolization of the end vessel may terminate the hemorrhage. However, a distal pancreatectomy—surgery to remove of the tail of the pancreas—may be required to stop the hemorrhage.
Frey's procedure is a surgical technique used in the treatment of chronic pancreatitis in which the diseased portions of the pancreas head are cored out. A lateral pancreaticojejunostomy (LRLPJ) is then performed in which a loop of the jejunum is then mobilized and attached over the exposed pancreatic duct to allow better drainage of the pancreas, including its head.
Pancreatitis is a common condition in cats and dogs. Pancreatitis is inflammation of the pancreas that can occur in two very different forms. Acute pancreatitis is sudden, while chronic pancreatitis is characterized by recurring or persistent form of pancreatic inflammation. Cases of both can be considered mild or severe. It is currently undecided whether chronic pancreatitis is a distinct disease or a form of acute pancreatitis. Other forms such as auto-immune and hereditary pancreatitis are presumed to occur but there existence has not been proven.
Pancreatic abscess is a late complication of acute necrotizing pancreatitis, occurring more than 4 weeks after the initial attack. A pancreatic abscess is a collection of pus resulting from tissue necrosis, liquefaction, and infection. It is estimated that approximately 3% of the patients with acute pancreatitis will develop an abscess.
A pancreatic injury is some form of trauma sustained by the pancreas. The injury can be sustained through either blunt forces, such as a motor vehicle accident, or penetrative forces, such as that of a gunshot wound. The pancreas is one of the least commonly injured organs in abdominal trauma.
Cystogastrostomy is a surgery to create an opening between a pancreatic pseudocyst and the stomach when the cyst is in a suitable position to be drained into the stomach. This conserves pancreatic juices that would otherwise be lost. This surgery is performed by a pancreatic surgeon to avoid a life-threatening rupture of the pancreatic pseudocyst.

Choledochoduodenostomy (CDD) is a surgical procedure to create an anastomosis, a surgical connection, between the common bile duct (CBD) and an alternative portion of the duodenum. In healthy individuals, the CBD meets the pancreatic duct at the ampulla of Vater, which drains via the major duodenal papilla to the second part of duodenum. In cases of benign conditions such as narrowing of the distal CBD or recurrent CBD stones, performing a CDD provides the diseased patient with CBD drainage and decompression. A side-to-side anastomosis is usually performed.
References
- ↑ Howell JG, Johnson LW, Sehon JK, Lee WC (2001). "Surgical management for chronic pancreatitis". The American Surgeon. 67 (5): 487–90. PMID 11379656.
- ↑ Bosmia, AN; Christein, JD (August 2017). "Charles Bernard Puestow (1902-1973): American surgeon and commander of the 27th Evacuation Hospital during the Second World War". Journal of Medical Biography. 25 (3): 147–152. doi:10.1177/0967772015608052. PMID 26508621. S2CID 6631023.