Dilationand curettage (D&C) refers to the dilation of the cervix and surgical removal of sections and or layers of the lining of the uterus and or contents of the uterus such as an unwanted fetus, remains of a non viable fetus, retained placenta after birth or abortion as well as any abnormal tissue which may be in the uterus causing abnormal cycles by scraping and scooping (curettage). It is a gynecologic procedure used for treatment and removal as well as diagnostic and therapeutic purposes, and is the most commonly used method for first trimester abortion or miscarriage.

The uterus or womb is the organ in the reproductive system of most female mammals, including humans, that accommodates the embryonic and fetal development of one or more embryos until birth. The uterus is a hormone-responsive sex organ that contains glands in its lining that secrete uterine milk for embryonic nourishment.
Gynecologic hemorrhage represents excessive bleeding of the female reproductive system. Such bleeding could be visible or external, namely bleeding from the vagina, or it could be internal into the pelvic cavity or form a hematoma. Normal menstruation is not considered a gynecologic hemorrhage, as it is not excessive. Hemorrhage associated with a pregnant state or during delivery is an obstetrical hemorrhage.

Hysterectomy is the surgical removal of the uterus and cervix. Supracervical hysterectomy refers to removal of the uterus while the cervix is spared. These procedures may also involve removal of the ovaries (oophorectomy), fallopian tubes (salpingectomy), and other surrounding structures. The term “partial” or “total” hysterectomy are lay-terms that incorrectly describe the addition or omission of oophorectomy at the time of hysterectomy. These procedures are usually performed by a gynecologist. Removal of the uterus renders the patient unable to bear children and has surgical risks as well as long-term effects, so the surgery is normally recommended only when other treatment options are not available or have failed. It is the second most commonly performed gynecological surgical procedure, after cesarean section, in the United States. Nearly 68 percent were performed for conditions such as endometriosis, irregular bleeding, and uterine fibroids. It is expected that the frequency of hysterectomies for non-malignant indications will continue to fall given the development of alternative treatment options.

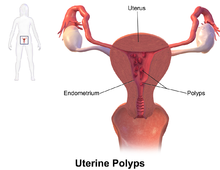
A polyp is an abnormal growth of tissue projecting from a mucous membrane. If it is attached to the surface by a narrow elongated stalk, it is said to be pedunculated; if it is attached without a stalk, it is said to be sessile. Polyps are commonly found in the colon, stomach, nose, ear, sinus(es), urinary bladder, and uterus. They may also occur elsewhere in the body where there are mucous membranes, including the cervix, vocal folds, and small intestine. Some polyps are tumors (neoplasms) and others are non-neoplastic, for example hyperplastic or dysplastic, which are benign. The neoplastic ones are usually benign, although some can be pre-malignant, or concurrent with a malignancy.

Uterine cancer, also known as womb cancer, includes two types of cancer that develop from the tissues of the uterus. Endometrial cancer forms from the lining of the uterus, and uterine sarcoma forms from the muscles or support tissue of the uterus. Endometrial cancer accounts for approximately 90% of all uterine cancers in the United States. Symptoms of endometrial cancer include changes in vaginal bleeding or pain in the pelvis. Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the vagina.
Heavy menstrual bleeding (HMB), previously known as menorrhagia or hematomunia, is a menstrual period with excessively heavy flow. It is a type of abnormal uterine bleeding (AUB).
Abnormal uterine bleeding (AUB), also known as atypical vaginal bleeding (AVB), is vaginal bleeding from the uterus that is abnormally frequent, lasts excessively long, is heavier than normal, or is irregular. The term dysfunctional uterine bleeding was used when no underlying cause was present. Vaginal bleeding during pregnancy is excluded. Iron deficiency anemia may occur and quality of life may be negatively affected.

Asherman's syndrome (AS) is an acquired uterine condition that occurs when scar tissue (adhesions) forms inside the uterus and/or the cervix. It is characterized by variable scarring inside the uterine cavity, where in many cases the front and back walls of the uterus stick to one another. AS can be the cause of menstrual disturbances, infertility, and placental abnormalities. Although the first case of intrauterine adhesion was published in 1894 by Heinrich Fritsch, it was only after 54 years that a full description of Asherman syndrome was carried out by Joseph Asherman. A number of other terms have been used to describe the condition and related conditions including: uterine/cervical atresia, traumatic uterine atrophy, sclerotic endometrium, and endometrial sclerosis.

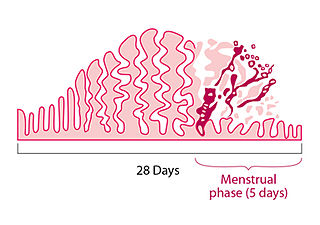
Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus (endometrium) atypically located among the cells of the uterine wall (myometrium), as a result, thickening of the uterus occurs. As well as being misplaced in patients with this condition, endometrial tissue is completely functional. The tissue thickens, sheds and bleeds during every menstrual cycle.

Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reproductive system, such as abnormal uterine bleeding.

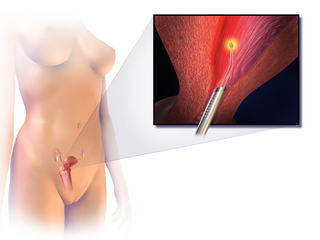
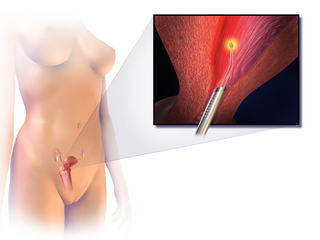
Hysteroscopy is the inspection of the uterine cavity by endoscopy with access through the cervix. It allows for the diagnosis of intrauterine pathology and serves as a method for surgical intervention.
Endometrial ablation is a surgical procedure that is used to remove (ablate) or destroy the endometrial lining of the uterus. The goal of the procedure is to decrease the amount of blood loss during menstrual periods. Endometrial ablation is most often employed in people with excessive menstrual bleeding, who do not wish to undergo a hysterectomy, following unsuccessful medical therapy.
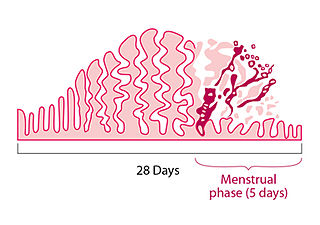
A menstrual disorder is characterized as any abnormal condition with regards to a woman's menstrual cycle. There are many different types of menstrual disorders that vary with signs and symptoms, including pain during menstruation, heavy bleeding, or absence of menstruation. Normal variations can occur in menstrual patterns but generally menstrual disorders can also include periods that come sooner than 21 days apart, more than 3 months apart, or last more than 10 days in duration. Variations of the menstrual cycle are mainly caused by the immaturity of the hypothalamic-pituitary-ovarian (HPO) axis, and early detection and management is required in order to minimize the possibility of complications regarding future reproductive ability.

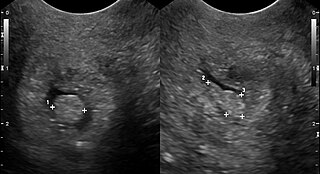
The endometrial biopsy is a medical procedure that involves taking a tissue sample of the lining of the uterus. The tissue subsequently undergoes a histologic evaluation which aids the physician in forming a diagnosis.

Hematometra is a medical condition involving collection or retention of blood in the uterus. It is most commonly caused by an imperforate hymen or a transverse vaginal septum.
A cervical polyp is a common benign polyp or tumour on the surface of the cervical canal. They can cause irregular menstrual bleeding but often show no symptoms. Treatment consists of simple removal of the polyp and prognosis is generally good. About 1% of cervical polyps will show neoplastic change which may lead to cancer. They are most common in post-menarche, pre-menopausal women who have been pregnant.
Hypomenorrhea or hypomenorrhoea, also known as short or scanty periods, is extremely light menstrual blood flow. It is the opposite of heavy periods or hypermenorrhea which is more properly called menorrhagia.
Uterine clear-cell carcinoma (CC) is a rare form of endometrial cancer with distinct morphological features on pathology; it is aggressive and has high recurrence rate. Like uterine papillary serous carcinoma CC does not develop from endometrial hyperplasia and is not hormone sensitive, rather it arises from an atrophic endometrium. Such lesions belong to the type II endometrial cancers.
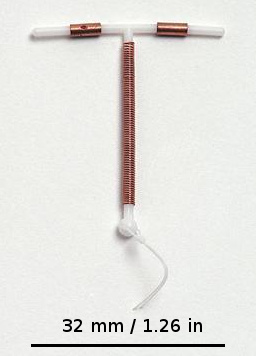
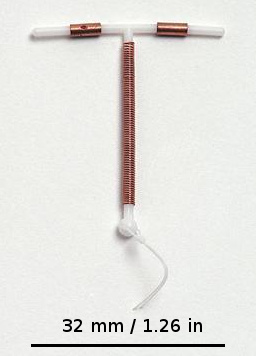
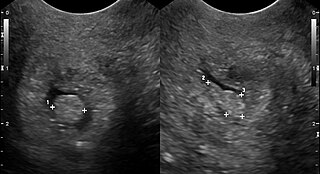
An intrauterine device (IUD), also known as intrauterine contraceptive device or coil, is a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. IUDs are a form of long-acting reversible birth control (LARC).