Diagnosis
| | This section is empty. You can help by adding to it. (September 2020) |
| Urethrocele | |
|---|---|
| Other names | Cystourethrocele |
| Pronunciation | |
| Specialty | Gynecology |
A urethrocele is the prolapse of the female urethra into the vagina. Weakening of the tissues that hold the urethra in place may cause it to protrude into the vagina. [3] [4] Urethroceles often occur with cystoceles (involving the urinary bladder as well as the urethra). [5] In this case, the term used is cystourethrocele. [6] [7]
There are often no symptoms associated with a urethrocele. [3] When present, symptoms include stress incontinence, increased urinary frequency, and urinary retention (difficulty in emptying the bladder). [3] [6] Pain during sexual intercourse may also occur. [5]
Where a urethrocele causes difficulty in urinating, this can lead to cystitis. [3]
Urethroceles can often result as a result of damage to the supporting structures of the pelvic floor. Urethroceles can form after treatment for gynecological cancers. [8] Urethroceles are often caused by childbirth, the movement of the baby through the vagina causing damage to the surrounding tissues. [5] When they occur in women who have never had children, they may be the result of a congenital weakness in the tissues of the pelvic floor. [9]
| | This section is empty. You can help by adding to it. (September 2020) |
A urethrocele can be treated surgically. [4]
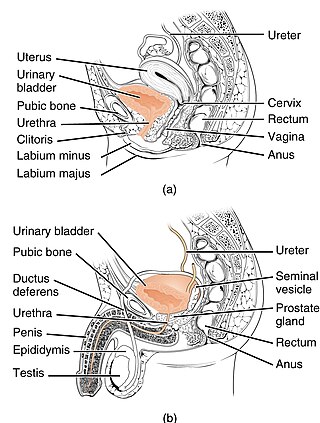
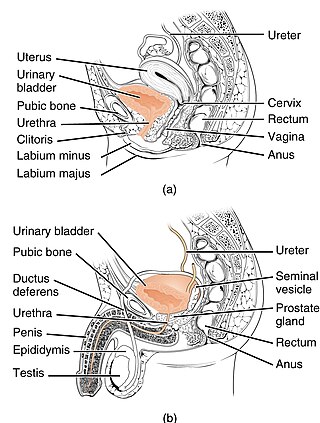
The urethra is a tube that connects the urinary bladder to the urinary meatus for the removal of urine from the body of both females and males. In human females and other primates, the urethra connects to the urinary meatus above the vagina, whereas in marsupials, the female's urethra empties into the urogenital sinus.
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis. UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse. People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.
In medicine, prolapse is a condition in which organs fall down or slip out of place. It is used for organs protruding through the vagina, rectum, or for the misalignment of the valves of the heart. A spinal disc herniation is also sometimes called "disc prolapse". Prolapse means "to fall out of place", from the Latin prolabi meaning "to fall out".
A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage and to treat pelvic organ prolapse to maintain the location of organs in the pelvic region. It can also be used to administer medications locally in the vagina or as a method of contraception.

The pelvic floor or pelvic diaphragm is a muscular partition separating the pelvic cavity (above), and perineal region (below). It is formed by the levator ani muscle and coccygeus muscle, and associated connective tissue.
In gynecology, a rectocele or posterior vaginal wall prolapse results when the rectum bulges (herniates) into the vagina. Two common causes of this defect are childbirth and hysterectomy. Rectocele also tends to occur with other forms of pelvic organ prolapse, such as enterocele, sigmoidocele and cystocele.

Vaginoplasty is any surgical procedure that results in the construction or reconstruction of the vagina. It is a type of genitoplasty. Pelvic organ prolapse is often treated with one or more surgeries to repair the vagina. Sometimes a vaginoplasty is needed following the treatment or removal of malignant growths or abscesses in order to restore a normal vaginal structure and function. Surgery to the vagina is done to correct congenital defects to the vagina, urethra and rectum. It will correct protrusion of the urinary bladder into the vagina (cystocele) and protrusion of the rectum (rectocele) into the vagina. Often, a vaginoplasty is performed to repair the vagina and its attached structures due to trauma or injury. Labiaplasty, which alters the appearance of the vulva, can be performed as a discrete surgery, or as a subordinate procedure within a vaginoplasty.

Pelvic floor dysfunction is a term used for a variety of disorders that occur when pelvic floor muscles and ligaments are impaired. The condition affects up to 50 percent of women who have given birth. Although this condition predominantly affects women, up to 16 percent of men are affected as well. Symptoms can include pelvic pain, pressure, pain during sex, urinary incontinence (UI), overactive bladder, bowel incontinence, incomplete emptying of feces, constipation, myofascial pelvic pain and pelvic organ prolapse. When pelvic organ prolapse occurs, there may be visible organ protrusion or a lump felt in the vagina or anus.

The cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's bladder bulges into her vagina. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence, or frequent urination. Complications may include recurrent urinary tract infections and urinary retention. Cystocele and a prolapsed urethra often occur together and is called a cystourethrocele. Cystocele can negatively affect quality of life.

Pelvic organ prolapse (POP) is characterized by descent of pelvic organs from their normal positions into the vagina. In women, the condition usually occurs when the pelvic floor collapses after gynecological cancer treatment, childbirth or heavy lifting. Injury incurred to fascia membranes and other connective structures can result in cystocele, rectocele or both. Treatment can involve dietary and lifestyle changes, physical therapy, or surgery.

Pelvic exenteration is a radical surgical treatment that removes all organs from a person's pelvic cavity. It is used to treat certain advanced or recurrent cancers. The urinary bladder, urethra, rectum, and anus are removed. In women, the vagina, cervix, uterus, Fallopian tubes, ovaries and, in some cases, the vulva are removed. In men, the prostate is removed. The procedure leaves the person with a permanent colostomy and urinary diversion.

Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.

Uterine prolapse is a form of pelvic organ prolapse in which the uterus and a portion of the upper vagina protrude into the vaginal canal and, in severe cases, through the opening of the vagina. It is most often caused by injury or damage to structures that hold the uterus in place within the pelvic cavity. Symptoms may include vaginal fullness, pain with sexual intercourse, difficulty urinating, and urinary incontinence. Risk factors include older age, pregnancy, vaginal childbirth, obesity, chronic constipation, and chronic cough. Prevalence, based on physical exam alone, is estimated to be approximately 14%.

The urethral sphincters are two muscles used to control the exit of urine in the urinary bladder through the urethra. The two muscles are either the male or female external urethral sphincter and the internal urethral sphincter. When either of these muscles contracts, the urethra is sealed shut.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.
Sigmoidocele refers to a condition where the sigmoid colon descends (prolapses) into the lower pelvic cavity. This can obstruct the rectum and cause symptoms of obstructed defecation.
Vaginal rugae are structures of the vagina that are transverse ridges formed out of the supporting tissues and vaginal epithelium in females. Some conditions can cause the disappearance of vaginal rugae and are usually associated with childbirth and prolapse of pelvic structures. The rugae contribute to the resiliency and elasticity of the vagina and its ability to distend and return to its previous state. These structures not only allow expansions and an increase in surface area of the vaginal epithelium, they provide the space necessary for the vaginal microbiota. The shape and structure of the rugae are supported and maintained by the lamina propria of the vagina and the anterior and posterior rugae.

Vaginal cysts are uncommon benign cysts that develop in the vaginal wall. The type of epithelial tissue lining a cyst is used to classify these growths. They can be congenital. They can present in childhood and adulthood. The most common type is the squamous inclusion cyst. It develops within vaginal tissue present at the site of an episiotomy or other vaginal surgical sites. In most instances they do not cause symptoms and present with few or no complications. A vaginal cyst can develop on the surface of the vaginal epithelium or in deeper layers. Often, they are found by the woman herself and as an incidental finding during a routine pelvic examination. Vaginal cysts can mimic other structures that protrude from the vagina such as a rectocele and cystocele. Some cysts can be distinguished visually but most will need a biopsy to determine the type. Vaginal cysts can vary in size and can grow as large as 7 cm. Other cysts can be present on the vaginal wall though mostly these can be differentiated. Vaginal cysts can often be palpated (felt) by a clinician. Vaginal cysts are one type of vaginal mass, others include cancers and tumors. The prevalence of vaginal cysts is uncertain since many go unreported but it is estimated that 1 out of 200 women have a vaginal cyst. Vaginal cysts may initially be discovered during pregnancy and childbirth. These are then treated to provide an unobstructed delivery of the infant. Growths that originate from the urethra and other tissue can present as cysts of the vagina.
Transvaginal mesh, also known as vaginal mesh implant, is a net-like surgical tool that is used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI) among female patients. The surgical mesh is placed transvaginally to reconstruct weakened pelvic muscle walls and to support the urethra or bladder.