Related Research Articles

Allergies, also known as allergic diseases, are a number of conditions caused by hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include hay fever, food allergies, atopic dermatitis, allergic asthma, and anaphylaxis. Symptoms may include red eyes, an itchy rash, sneezing, a runny nose, shortness of breath, or swelling. Food intolerances and food poisoning are separate conditions.
An allergen is a type of antigen that produces an abnormally vigorous immune response in which the immune system fights off a perceived threat that would otherwise be harmless to the body. Such reactions are called allergies.

Allergic rhinitis, of which the seasonal type is called hay fever, is a type of inflammation in the nose that occurs when the immune system overreacts to allergens in the air. Signs and symptoms include a runny or stuffy nose, sneezing, red, itchy, and watery eyes, and swelling around the eyes. The fluid from the nose is usually clear. Symptom onset is often within minutes following allergen exposure, and can affect sleep and the ability to work or study. Some people may develop symptoms only during specific times of the year, often as a result of pollen exposure. Many people with allergic rhinitis also have asthma, allergic conjunctivitis, or atopic dermatitis.
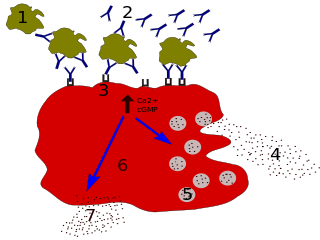
Immunoglobulin E (IgE) is a type of antibody that has been found only in mammals. IgE is synthesised by plasma cells. Monomers of IgE consist of two heavy chains and two light chains, with the ε chain containing four Ig-like constant domains (Cε1–Cε4). IgE is thought to be an important part of the immune response against infection by certain parasitic worms, including Schistosoma mansoni, Trichinella spiralis, and Fasciola hepatica. IgE is also utilized during immune defense against certain protozoan parasites such as Plasmodium falciparum. IgE may have evolved as a defense to protect against venoms.

A food allergy is an abnormal immune response to food. The symptoms of the allergic reaction may range from mild to severe. They may include itchiness, swelling of the tongue, vomiting, diarrhea, hives, trouble breathing, or low blood pressure. This typically occurs within minutes to several hours of exposure. When the symptoms are severe, it is known as anaphylaxis. A food intolerance and food poisoning are separate conditions, not due to an immune response.
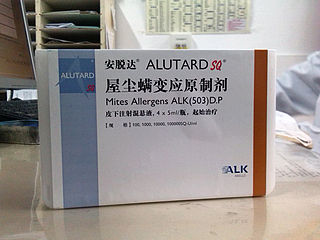
Allergen immunotherapy, also known as desensitization or hypo-sensitization, is a medical treatment for environmental allergies, such as insect bites, and asthma. Immunotherapy involves exposing people to larger and larger amounts of allergen in an attempt to change the immune system's response.

Peanut allergy is a type of food allergy to peanuts. It is different from tree nut allergies, because peanuts are legumes and not true nuts. Physical symptoms of allergic reaction can include itchiness, hives, swelling, eczema, sneezing, asthma attack, abdominal pain, drop in blood pressure, diarrhea, and cardiac arrest. Anaphylaxis may occur. Those with a history of asthma are more likely to be severely affected.

Soy allergy is a type of food allergy. It is a hypersensitivity to ingesting compounds in soy, causing an overreaction of the immune system, typically with physical symptoms, such as gastrointestinal discomfort, respiratory distress, or a skin reaction. Soy is among the eight most common foods inducing allergic reactions in children and adults. It has a prevalence of about 0.3% in the general population.
Allergic bronchopulmonary aspergillosis (ABPA) is a condition characterised by an exaggerated response of the immune system to the fungus Aspergillus. It occurs most often in people with asthma or cystic fibrosis. Aspergillus spores are ubiquitous in soil and are commonly found in the sputum of healthy individuals. A. fumigatus is responsible for a spectrum of lung diseases known as aspergilloses.
Nambudripad's Allergy Elimination Techniques (NAET) is a form of alternative medicine which proponents claim can treat allergies and related disorders. The techniques were devised by Devi Nambudripad, a California-based chiropractor and acupuncturist, in 1983, drawing on a combination of ideas from applied kinesiology, acupuncture, acupressure, nutritional management, and chiropractic methods.

Milk allergy is an adverse immune reaction to one or more proteins in cow's milk. When allergy symptoms occur, they can occur rapidly or have a gradual onset. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine among other measures. The latter can take hours to days to appear, with symptoms including atopic dermatitis, inflammation of the esophagus, enteropathy involving the small intestine and proctocolitis involving the rectum and colon.

Egg allergy is an immune hypersensitivity to proteins found in chicken eggs, and possibly goose, duck, or turkey eggs. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus.
Skin allergy testing comprises a range of methods for medical diagnosis of allergies that attempts to provoke a small, controlled, allergic response.
Phadia develops, manufactures and markets blood test systems to support the clinical diagnosis and monitoring of allergy, asthma and autoimmune diseases. The company is headquartered in Uppsala, Sweden. It has been owned by Thermo Fisher Scientific since 2011.
Allergy testing can help confirm or rule out allergies and consequently reduce adverse reactions and limit unnecessary avoidance and medications.

Alain L. de Weck,, was a Swiss immunologist and allergist. His main scientific contributions were in the area of characterization and prevention of drug allergy. He was the founding director of the Institute of Clinical Immunology at the University of Bern from 1971 to 1993 and authored or co-authored over 600 peer-reviewed publications. He is the recipient of a number of patents that led to commercial allergy products and services. He served as president of international scientific organizations such as the International Union of Immunological Societies (IUIS) and the International Association for Allergy and Clinical Immunology (IAACI) and was founder and later CEO of the Centre Médical des Grand-Places (CMG) company, acquired by Heska of Fort Collins in 1997. In later years he continued his research at the University of Navarra in Spain and wrote on a wide range of topics such as the distinction between science and pseudo-science, the emergence of genetically modified organisms (GMOs) and comparative health care policy.
Alpha-gal allergy — or mammalian meat allergy (MMA) — is a type of meat allergy characterized by a delayed onset of symptoms after ingesting mammalian meat and resulting from past exposure to tick bites. It was first reported in 2002. Symptoms of the allergy include rash, hives, nausea or vomiting, difficulty breathing, drop in blood pressure, dizziness or faintness and severe stomach pain.
Cross-reactive carbohydrate determinants (CCDs) play a role in the context of allergy diagnosis. The terms CCD or CCDs describe protein-linked carbohydrate structures responsible for the phenomenon of cross-reactivity of sera from allergic patients towards a wide range of allergens from plants and insects. In serum-based allergy diagnosis, antibodies of the IgE class directed against CCDs therefore give the impression of polysensitization. Anti-CCD IgE, however, does not seem to elicit clinical symptoms. Diagnostic results caused by CCDs are therefore regarded as false positives.
Rice allergy is a type of food allergy. People allergic to rice react to some rice proteins after they eat rice or breathe in rice steam. Although some reactions might lead to severe health problems, doctors can diagnose rice allergy with many methods and help allergic people to avoid reactions.

Shellfish allergy is among the most common food allergies. "Shellfish" is a colloquial and fisheries term for aquatic invertebrates used as food, including various species of molluscs such as clams, mussels, oysters and scallops, crustaceans such as shrimp, lobsters and crabs, and cephalopods such as squid and octopus. Shellfish allergy is an immune hypersensitivity to proteins found in shellfish. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus. Shellfish is one of the eight common food allergens, responsible for 90% of allergic reactions to foods: cow's milk, eggs, wheat, shellfish, peanuts, tree nuts, fish, and soy beans.
References
- ↑ NIH Guidelines for the Diagnosis and Management of Food Allergy in the United States. Report of the NIAID- Sponsored Expert Panel, 2010, NIH Publication no. 11-7700.
- ↑ Cox, L. Overview of Serological-Specific IgE Antibody Testing in Children. Pediatric Allergy and Immunology. 2011.
- ↑ Hamilton R et al. Proficiency Survey-Based Evaluation of Clinical Total and Allergen-Specific IgE Assay Performance. Arch Pathol Lab Med. 2010; 134: 975–982
- ↑ UpToDate (http://www.uptodate.com/contents/overview-of-skin-testing-for-allergic-disease?source=search_result&search=skin+testing&selectedTitle=1~150)
- ↑ Chinoy B, Yee E, Bahna SL. Skin testing versus radioallergosorbent testing for indoor allergens. Clin Mol Allergy. 2005 Apr 15;3(1):4.
- ↑ Holzweber, F. (2013). "Inhibition of IgE binding to cross-reactive carbohydrate determinants enhances diagnostic selectivity". Allergy. 68 (10): 1269–1277. doi:10.1111/all.12229. PMC 4223978 . PMID 24107260.
- ↑ Boyce J et al. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of
- ↑ Wood R; et al. (2007). "Accuracy of IgE antibody laboratory results". Ann Allergy Asthma Immunol. 99 (1): 34–41. doi:10.1016/s1081-1206(10)60618-7. PMID 17650827.
- ↑ Wang J, Godbold JH, Sampson HA (2008). "Correlation of serum allergy (IgE) tests performed by different assay systems". J. Allergy Clin. Immunol. 121 (5): 1219–24. doi:10.1016/j.jaci.2007.12.1150. PMID 18243289.
- ↑ American Academy of Allergy, Asthma, and Immunology, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation , American Academy of Allergy, Asthma, and Immunology , retrieved August 14, 2012
{{citation}}: CS1 maint: multiple names: authors list (link) - ↑ Cox, L.; Williams, B.; Sicherer, S.; Oppenheimer, J.; Sher, L.; Hamilton, R.; Golden, D. (2008). "Pearls and pitfalls of allergy diagnostic testing: Report from the American College of Allergy, Asthma and Immunology/American Academy of Allergy, Asthma and Immunology Specific IgE Test Task Force". Annals of Allergy, Asthma & Immunology. 101 (6): 580–592. doi:10.1016/S1081-1206(10)60220-7. PMID 19119701.
- ↑ WebMD > Medical Dictionary > radioallergosorbent test (RAST) Citing: Stedman’s Medical Dictionary 28th Edition. Copyright 2006
- ↑ NIAID-Sponsored Expert Panel (December 2010). "Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel". The Journal of Allergy and Clinical Immunology. 126 (6): S1–S58. doi:10.1016/j.jaci.2010.10.007. PMC 4241964 . PMID 21134576 . Retrieved 30 August 2012.