Related Research Articles

The AIDS epidemic, caused by HIV, found its way to the United States between the 1970s and 1980s, but was first noticed after doctors discovered clusters of Kaposi's sarcoma and pneumocystis pneumonia in homosexual men in Los Angeles, New York City, and San Francisco in 1981. Treatment of HIV/AIDS is primarily via the use of multiple antiretroviral drugs, and education programs to help people avoid infection.
Men who have sex with men (MSM) are men who engage in sexual activity with other men, regardless of their sexual orientation or sexual identity. The term was created by epidemiologists in the 1990s, to better study and communicate the spread of sexually transmitted infections such as HIV/AIDS between all sexually active males, not strictly those identifying as gay, bisexual, pansexual or various other sexualities, but also for example male prostitutes. The term is often used in medical literature and social research to describe such men as a group. It does not describe any specific kind of sexual activity, and which activities are covered by the term depends on context. The alternative term "males who have sex with males" is sometimes considered more accurate in cases where those described may not be legal adults.

The global pandemic of HIV/AIDS began in 1981, and is an ongoing worldwide public health issue. According to the World Health Organization (WHO), by 2023, HIV/AIDS had killed approximately 40.4 million people, and approximately 39 million people were infected with HIV globally. Of these, 29.8 million people (75%) are receiving antiretroviral treatment. There were about 630,000 deaths from HIV/AIDS in 2022. The 2015 Global Burden of Disease Study estimated that the global incidence of HIV infection peaked in 1997 at 3.3 million per year. Global incidence fell rapidly from 1997 to 2005, to about 2.6 million per year. Incidence of HIV has continued to fall, decreasing by 23% from 2010 to 2020, with progress dominated by decreases in Eastern Africa and Southern Africa. As of 2023, there are about 1.3 million new infections of HIV per year globally.

Lesbian, gay, bisexual, and transgender (LGBTQ) people in Jamaica face legal and social issues not experienced by heterosexual and gender-conforming people. Consensual sexual intercourse between same-sex partners is legally punishable by up to 10 years of imprisonment in the country.

Lesbian, gay, bisexual, and transgender (LGBT) people in Kenya face significant challenges not experienced by non-LGBTQ residents. Sodomy is a felony per Section 162 of the Kenyan Penal Code, punishable by 21 years' imprisonment, and any sexual practices are a felony under section 165 of the same statute, punishable by five years' imprisonment. On 24 May 2019, the High Court of Kenya refused an order to declare sections 162 and 165 unconstitutional. The state does not recognise any relationships between persons of the same sex; same-sex marriage is banned under the Kenyan Constitution since 2010. There are no explicit protections against discrimination on the basis of sexual orientation and gender identity. Adoption is restricted to heterosexual couples only.

HIV/AIDS in India is an epidemic. The National AIDS Control Organisation (NACO) estimated that 3.14 million people lived with HIV/AIDS in India in 2023. Despite being home to the world's third-largest population of persons with HIV/AIDS, the AIDS prevalence rate in India is lower than that of many other countries. In 2016, India's AIDS prevalence rate stood at approximately 0.30%—the 80th highest in the world. Treatment of HIV/AIDS is via a combination of antiretroviral drugs and education programs to help people avoid infection.
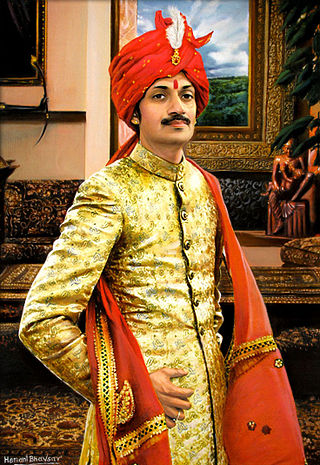
Manvendra Singh Gohil is an Indian prince, being the son and probable heir of the honorary Maharaja of Rajpipla. He is considered to be the first openly gay prince in the world, and he is known for being one of India's foremost LGBT activists. He runs a charity, the Lakshya Trust, which works with the LGBT community.

Lesbian, gay, bisexual, transgender, and queer (LGBTQ) rights in Argentina rank among the highest in the world. Upon legalising same-sex marriage on 15 July 2010, Argentina became the first country in Latin America, the second in the Americas, and the tenth in the world to do so. Following Argentina's transition to a democracy in 1983, its laws have become more inclusive and accepting of LGBT people, as has public opinion.
The history of HIV/AIDS in Australia is distinctive, as Australian government bodies recognised and responded to the AIDS pandemic relatively swiftly, with the implementation of effective disease prevention and public health programs, such as needle and syringe programs (NSPs). As a result, despite significant numbers of at-risk group members contracting the virus in the early period following its discovery, Australia achieved and has maintained a low rate of HIV infection in comparison to the rest of the world.
With less than 0.1 percent of the population estimated to be HIV-positive, Bangladesh is a low HIV-prevalence country.

68 Pages is a 2007 Indian film about an HIV/AIDS counselor and five of her clients who are from marginalized communities. The film is directed by Sridhar Rangayan and produced by Humsafar Trust in association with Solaris Pictures. It had its world premiere at the International Film Festival of Kerala and screened at several international film festivals. It won the Silver Remi award at WorldFest Houston International Film Festival 2008, USA. The film was also screened in the Pink Ribbon Express, a National AIDS Control Organisation initiative.

Avert is an international charity that uses digital communications to increase health literacy on HIV and sexual health, among those most affected in areas of greatest need, in order to reduce new infections and improve health and well-being.

Lesbian, gay, bisexual, and transgender (LGBT) rights in Mauritius have expanded in the 21st century, although LGBT Mauritians may still face legal difficulties not experienced by non-LGBTQ residents. Prior to 2023, sodomy was criminalized by Section 250 of the Criminal Code. However, Mauritius fully decriminalized homosexuality in October 2023. Although same-sex marriage is not recognized in Mauritius, LGBT people are broadly protected from discrimination in areas such as employment and the provision of goods and services, making it one of the few African countries to have such protections for LGBT people. The Constitution of Mauritius guarantees the right of individuals to a private life.
The first HIV/AIDS case in Malaysia made its debut in 1986. Since then, HIV/AIDS has become one of the country's most serious health and development challenges. As of 2020, the Ministry of Health estimated that 87 per cent of an estimated 92,063 people living with HIV (PLHIV) in Malaysia were aware of their status, 58 per cent of reported PLHIV received antiretroviral therapy, and 85 per cent of those on antiretroviral treatment became virally suppressed. Despite making positive progress, Malaysia still fell short of meeting the global 2020 HIV goals of 90-90-90, with a scorecard of 87-58-85.
The Naz Foundation (India) Trust is a non-governmental organisation (NGO) in that country that works on HIV/AIDS and sexual health. It is based in the Indian capital of New Delhi.

The National AIDS Control Organisation (NACO), established in 1992 is a division of India's Ministry of Health and Family Welfare that provides leadership to HIV/AIDS control programme in India through 35 HIV/AIDS Prevention and Control Societies, and is "the nodal organisation for formulation of policy and implementation of programs for prevention and control of HIV/AIDS in India.".

The majority of the countries of the Commonwealth of Nations, formerly known as the British Commonwealth, still criminalise sexual acts between consenting adults of the same sex and other forms of sexual orientation, gender identity and expression. Homosexual activity remains a criminal offence in 29 of the 56 sovereign states of the Commonwealth; and legal in only 26.
Humsafar Trust is an NGO in Mumbai that promotes LGBT rights. Founded by Ashok Row Kavi, Suhail Abbasi, and Sridhar Rangayan in 1994, it is one of the largest and most active of such organisations in India. It provides counselling, advocacy and healthcare to LGBT communities and has helped reduce violence, discrimination and stigma against them. Humsafar Trust is the convenor member of Integrated Network for Sexual Minorities (INFOSEM).

Founded in 1999, Alliance India is a non-governmental organisation operating in partnership with civil society, government and communities to support sustained responses to HIV in India that protect rights and improve health. Complementing the Indian national programme, we build capacity, provide technical support and advocate to strengthen the delivery of effective, innovative, community-based HIV programmes to vulnerable populations: sex workers, men who have sex with men (MSM), transgender people, hijras, people who inject drugs (PWID), and people living with HIV.
The Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome Act, 2017, often shortened to the HIV/AIDS Prevention Act, is an act of the Parliament of India that provides for controlling and preventing of HIV/AIDS and securing the rights of individuals diagnosed with HIV/AIDS. The bill for the act was introduced in the Rajya Sabha on 11 February 2014 and was referred to a Standing Committee on 24 February 2014, which submitted its report on 29 April 2015. After few amendments to the original 2014 bill, it was passed by the Rajya Sabh on 21 March 2017 and the Lok Sabha on 11 April 2017. It received Presidential assent on 20 April 2017, and became effective from 10 September 2018. The HIV/AIDS Prevention Act originated from a draft bill submitted by Lawyers Collective, a non-governmental organization, to the National AIDS Control Organisation (NACO) in 2006. The act penalises propagation of hate against HIV/AIDS affected persons, ensures the right of HIV/AIDS affected minors to shared household, protects non-disclosure of HIV/AIDS status in the absence of court order and mandates informed consent to disclose HIV/AIDS positive identity, inter alia. However, civil society organisations and HIV/AIDS affected persons criticised the act on certain legal language issues, as it mandates the state to provide HIV/AIDS affected persons with medical services "as far as possible". This aspect was absent from the draft bill submitted to NACO.
References
- 1 2 U.S. Agency for International Development: Directory of Associations of People Living with HIV/Aids, July 2004 Archived 2012-01-27 at the Wayback Machine , accessed February 19, 2012
- ↑ Udaan Trust: Objective Archived 2013-10-07 at the Wayback Machine , accessed February 19, 2012
- ↑ Staff writer (June 24, 2002). "Udaan: Dedicated to problems of gays". The Times of India . Archived from the original on May 9, 2012. Retrieved February 19, 2012.
- ↑ Udaan Trust: Projects Archived 2012-03-22 at the Wayback Machine , accessed February 19, 2012
- ↑ Sumitra Deb Roy (June 23, 2011). "AIDS work by 8 NGOs in state dubbed failures". The Times of India . Archived from the original on February 1, 2014. Retrieved February 19, 2012.
- ↑ AVERT: USAID Team Visit, March 7, 2011 Archived April 26, 2011, at the Wayback Machine , accessed February 19, 2011
- ↑ "2 ambulances donated to Gurdaspur police". The Tribune (India). March 14, 2011. Retrieved February 19, 2012.