dextro-Transposition of the great arteries is a potentially life-threatening birth defect in the large arteries of the heart. The primary arteries are transposed.

Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this does not naturally close after birth it is referred to as a patent (open) foramen ovale (PFO). It is common in patients with a congenital atrial septal aneurysm (ASA).

A congenital heart defect (CHD), also known as a congenital heart anomaly, congenital cardiovascular malformation, and congenital heart disease, is a defect in the structure of the heart or great vessels that is present at birth. A congenital heart defect is classed as a cardiovascular disease. Signs and symptoms depend on the specific type of defect. Symptoms can vary from none to life-threatening. When present, symptoms are variable and may include rapid breathing, bluish skin (cyanosis), poor weight gain, and feeling tired. CHD does not cause chest pain. Most congenital heart defects are not associated with other diseases. A complication of CHD is heart failure.
A cyanotic heart defect is any congenital heart defect (CHD) that occurs due to deoxygenated blood bypassing the lungs and entering the systemic circulation, or a mixture of oxygenated and unoxygenated blood entering the systemic circulation. It is caused by structural defects of the heart such as right-to-left or bidirectional shunting, malposition of the great arteries, or any condition which increases pulmonary vascular resistance. The result may be the development of collateral circulation.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.
The Rastelli procedure is an open heart surgical procedure developed by Italian physician and cardiac surgery researcher, Giancarlo Rastelli, in 1967 at the Mayo Clinic, and involves using a pulmonary or aortic homograft conduit to relieve pulmonary obstruction in double outlet right ventricle with pulmonary stenosis.

Transposition of the great vessels (TGV) is a group of congenital heart defects involving an abnormal spatial arrangement of any of the great vessels: superior and/or inferior venae cavae, pulmonary artery, pulmonary veins, and aorta. Congenital heart diseases involving only the primary arteries belong to a sub-group called transposition of the great arteries (TGA), which is considered the most common congenital heart lesion that presents in neonates.
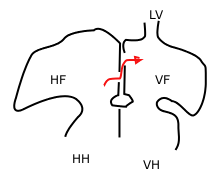
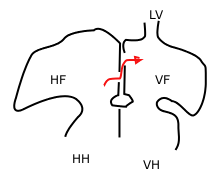
Levo-Transposition of the great arteries is an acyanotic congenital heart defect in which the primary arteries are transposed, with the aorta anterior and to the left of the pulmonary artery; the morphological left and right ventricles with their corresponding atrioventricular valves are also transposed.

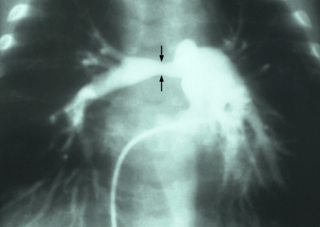
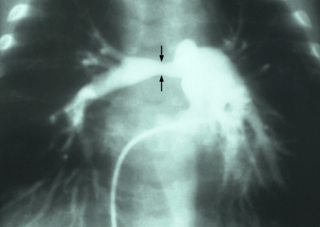
Balloon septostomy is the widening of a foramen ovale, patent foramen ovale (PFO), or atrial septal defect (ASD) via cardiac catheterization using a balloon catheter. This procedure allows a greater amount of oxygenated blood to enter the systemic circulation in some cases of cyanotic congenital heart defect (CHD).
An embolus, is described as a free-floating mass, located inside blood vessels that can travel from one site in the blood stream to another. An embolus can be made up of solid, liquid, or gas. Once these masses get "stuck" in a different blood vessel, it is then known as an "embolism." An embolism can cause ischemia—damage to an organ from lack of oxygen. A paradoxical embolism is a specific type of embolism in which the embolus travels from the right side of the heart to the left side of the heart and lodges itself in a blood vessel known as an artery. Thus, it is termed "paradoxical" because the embolus lands in an artery, rather than a vein.

Arterial switch operation (ASO) or arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries (d-TGA).
The foramen secundum, or ostium secundum is a foramen in the septum primum, a precursor to the interatrial septum of the human heart.
A cardiac shunt is a pattern of blood flow in the heart that deviates from the normal circuit of the circulatory system. It may be described as right-left, left-right or bidirectional, or as systemic-to-pulmonary or pulmonary-to-systemic. The direction may be controlled by left and/or right heart pressure, a biological or artificial heart valve or both. The presence of a shunt may also affect left and/or right heart pressure either beneficially or detrimentally.
The Mustard procedure was developed in 1963 by Dr. William Mustard at the Hospital for Sick Children in Toronto, Ontario, Canada.

Lutembacher's syndrome is a very rare form of congenital heart disease that affects one of the chambers of the heart as well as a valve. It is commonly known as both congenital atrial septal defect (ASD) and acquired mitral stenosis (MS). Congenital atrial septal defect refers to a hole being in the septum or wall that separates the two atria; this condition is usually seen in fetuses and infants. Mitral stenosis refers to mitral valve leaflets sticking to each other making the opening for blood to pass from the atrium to the ventricles very small. With the valve being so small, blood has difficulty passing from the left atrium into the left ventricle. Septal defects that may occur with Lutembacher's syndrome include: Ostium primum atrial septal defect or ostium secundum which is more prevalent.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.

Anomalous pulmonary venous connection is a congenital defect of the pulmonary veins.
Pulmonary artery stenosis (PAS) is a narrowing of the pulmonary artery. The pulmonary artery is a blood vessel moving blood from the right side of the heart to the lungs. This narrowing can be due to many causes, including infection during pregnancy, a congenital heart defect, a problem with blood clotting in childhood or early adulthood, or a genetic change.
The Senning procedure is an atrial switch heart operation performed to treat transposition of the great arteries. It is named after its inventor, the Swedish cardiac surgeon Åke Senning (1915–2000), also known for implanting the first permanent cardiac pacemaker in 1958.
William J. Rashkind was an American cardiologist. Rashkind worked at the Children's Hospital of Philadelphia. He is best known for his contributions to the treatment of congenital heart defects. He introduced the Rashkind balloon atrial septostomy to treat transposition of the great vessels.