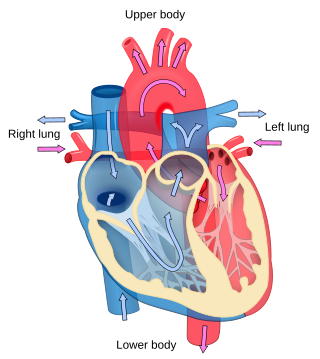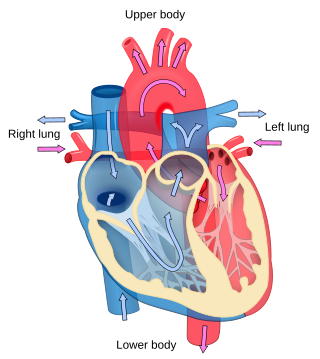
Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a sub-specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.
The diagnostic tests in cardiology are methods of identifying heart conditions associated with healthy vs. unhealthy, pathologic heart function.

Electrocardiography is the process of producing an electrocardiogram, a recording of the heart's electrical activity through repeated cardiac cycles. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including:

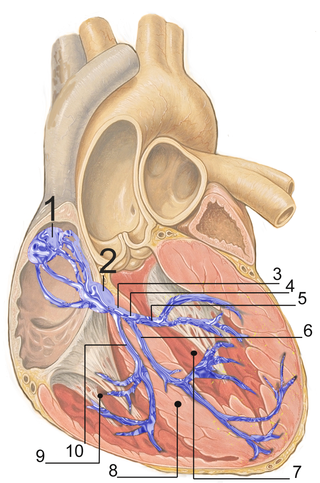
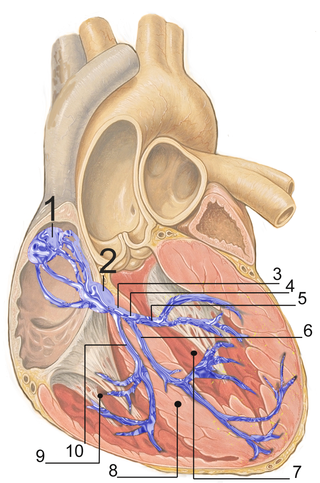
A pacemaker, also known as an artificial cardiac pacemaker, is an implanted medical device that generates electrical pulses delivered by electrodes to one or more of the chambers of the heart. Each pulse causes the targeted chamber(s) to contract and pump blood, thus regulating the function of the electrical conduction system of the heart.

Wolff–Parkinson–White syndrome (WPWS) is a disorder due to a specific type of problem with the electrical system of the heart involving an accessory pathway able to conduct electrical current between the atria and the ventricles, thus bypassing the atrioventricular node. About 60% of people with the electrical problem developed symptoms, which may include an abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, or syncope. Rarely, cardiac arrest may occur. The most common type of irregular heartbeat that occurs is known as paroxysmal supraventricular tachycardia.

Atrial flutter (AFL) is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate and is classified as a type of supraventricular tachycardia (SVT). Atrial flutter is characterized by a sudden-onset (usually) regular abnormal heart rhythm on an electrocardiogram (ECG) in which the heart rate is fast. Symptoms may include a feeling of the heart beating too fast, too hard, or skipping beats, chest discomfort, difficulty breathing, a feeling as if one's stomach has dropped, a feeling of being light-headed, or loss of consciousness.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.

Cardiac electrophysiology is a branch of cardiology and basic science focusing on the electrical activities of the heart. The term is usually used in clinical context, to describe studies of such phenomena by invasive (intracardiac) catheter recording of spontaneous activity as well as of cardiac responses to programmed electrical stimulation - clinical cardiac electrophysiology. However, cardiac electrophysiology also encompasses basic research and translational research components. Specialists studying cardiac electrophysiology, either clinically or solely through research, are known as cardiac electrophysiologists.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.

Catheter ablation is a procedure that uses radio-frequency energy or other sources to terminate or modify a faulty electrical pathway from sections of the heart of those who are prone to developing cardiac arrhythmias such as atrial fibrillation, atrial flutter and Wolff-Parkinson-White syndrome. If not controlled, such arrhythmias increase the risk of ventricular fibrillation and sudden cardiac arrest. The ablation procedure can be classified by energy source: radiofrequency ablation and cryoablation.
Lown–Ganong–Levine syndrome (LGL) is a pre-excitation syndrome of the heart. Those with LGL syndrome have episodes of abnormal heart racing with a short PR interval and normal QRS complexes seen on their electrocardiogram when in a normal sinus rhythm. LGL syndrome was originally thought to be due to an abnormal electrical connection between the atria and the ventricles, but is now thought to be due to accelerated conduction through the atrioventricular node in the majority of cases. The syndrome is named after Bernard Lown, William Francis Ganong, Jr., and Samuel A. Levine.
Clinical cardiac electrophysiology, is a branch of the medical specialty of cardiology concerned with the study and treatment of rhythm disorders of the heart. Cardiologists with expertise in this area are usually referred to as electrophysiologists. Electrophysiologists are trained in the mechanism, function, and performance of the electrical activities of the heart. Electrophysiologists work closely with other cardiologists and cardiac surgeons to assist or guide therapy for heart rhythm disturbances (arrhythmias). They are trained to perform interventional and surgical procedures to treat cardiac arrhythmia.
Pre-excitation syndrome is a heart condition in which part of the cardiac ventricles are activated too early. Pre-excitation is caused by an abnormal electrical connection or accessory pathway between or within the cardiac chambers. Pre-excitation may not cause any symptoms but may lead to palpitations caused by abnormal heart rhythms. It is usually diagnosed using an electrocardiogram, but may only be found during an electrophysiological study. The condition may not require any treatment at all, but symptoms can be controlled using medication or catheter ablation.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.

Michel Haïssaguerre is a French cardiologist and electrophysiologist. His investigations have been the basis for development of new markers and therapies for atrial and ventricular fibrillation.

Junctional ectopic tachycardia (JET) is a rare syndrome of the heart that manifests in patients recovering from heart surgery. It is characterized by cardiac arrhythmia, or irregular beating of the heart, caused by abnormal conduction from or through the atrioventricular node. In newborns and infants up to 6 weeks old, the disease may also be referred to as His bundle tachycardia or congenital JET.

Atrial fibrillation is an abnormal heart rhythm (arrhythmia) characterized by rapid and irregular beating of the atrial chambers of the heart. It often begins as short periods of abnormal beating, which become longer or continuous over time. It may also start as other forms of arrhythmia such as atrial flutter that then transform into AF.

Henrick Joan Joost Wellens, M.D., (1935–2020) was a Dutch cardiologist who is considered one of the founding fathers of clinical cardiac electrophysiology - a discipline which enables patients with cardiac arrhythmias to have catheter electrode mapping and ablation.

Arrhythmias, also known as cardiac arrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. Essentially, this is anything but normal sinus rhythm. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath, chest pain, or decreased level of consciousness. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.

Yaariv Khaykin is a Canadian cardiologist and a clinical researcher in the area of electrophysiology. He is the director of the Newmarket Electrophysiology Research Group at the Southlake Regional Health Centre. He has published research into complex ablation and pioneered cardiac ablation methods.