Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to generate pictures of the anatomy and the physiological processes inside the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to form images of the organs in the body. MRI does not involve X-rays or the use of ionizing radiation, which distinguishes it from computed tomography (CT) and positron emission tomography (PET) scans. MRI is a medical application of nuclear magnetic resonance (NMR) which can also be used for imaging in other NMR applications, such as NMR spectroscopy.

Myocarditis is defined as inflammation of the myocardium. Myocarditis can progress to inflammatory cardiomyopathy when there are associated ventricular remodeling and cardiac dysfunction due to chronic inflammation. Symptoms can include shortness of breath, chest pain, decreased ability to exercise, and an irregular heartbeat. The duration of problems can vary from hours to months. Complications may include heart failure due to dilated cardiomyopathy or cardiac arrest.
In cardiology, hibernating myocardium is a state when some segments of the myocardium exhibit abnormalities of contractile function. These abnormalities can be visualised with echocardiography, cardiac magnetic resonance imaging (CMR), nuclear medicine (PET) or ventriculography. Echocardiography: A wall motion abnormality at rest which improves during a low-dose dobutamine stress test is classified as "hibernating myocardium." Low dose dobutamine stimulates contractile function and thus helps to predict functional recovery after revascularization. Cardiac magnetic resonance: The most frequently used MR contrast agents based on Gd-chelates accumulate in the extracellular space which is increased in scarred myocardium. This leads to a signal increase which can be visualised with the "late gadolinium enhancement technique." This is probably the most accurate way to visualise scarred myocardium. An alternative (or additional) technique with CMR is the use of low dose dobutamine similar to echocardiography. PET: The finding of a perfusion or metabolic mismatch between PET-FDG and PET-NH3 is indicative of decreased metabolism. The wall of the affected segments is hypo-, a-, or dyskinetic.

Coronary thrombosis is defined as the formation of a blood clot inside a blood vessel of the heart. This blood clot may then restrict blood flow within the heart, leading to heart tissue damage, or a myocardial infarction, also known as a heart attack.
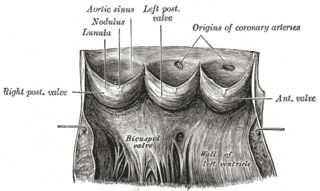
Aneurysm of the aortic sinus, also known as the sinus of Valsalva, is a rare abnormality of the aorta, the largest artery in the body. The aorta normally has three small pouches that sit directly above the aortic valve, and an aneurysm of one of these sinuses is a thin-walled swelling. Aneurysms may affect the right (65–85%), non-coronary (10–30%), or rarely the left coronary sinus. These aneurysms may not cause any symptoms but if large can cause shortness of breath, palpitations or blackouts. Aortic sinus aneurysms can burst or rupture into adjacent cardiac chambers, which can lead to heart failure if untreated.

Perfusion is the passage of fluid through the circulatory system or lymphatic system to an organ or a tissue, usually referring to the delivery of blood to a capillary bed in tissue. Perfusion may also refer to fixation via perfusion, used in histological studies. Perfusion is measured as the rate at which blood is delivered to tissue, or volume of blood per unit time per unit tissue mass. The SI unit is m3/(s·kg), although for human organs perfusion is typically reported in ml/min/g. The word is derived from the French verb perfuser, meaning to "pour over or through". All animal tissues require an adequate blood supply for health and life. Poor perfusion (malperfusion), that is, ischemia, causes health problems, as seen in cardiovascular disease, including coronary artery disease, cerebrovascular disease, peripheral artery disease, and many other conditions.

Left ventricular hypertrophy (LVH) is thickening of the heart muscle of the left ventricle of the heart, that is, left-sided ventricular hypertrophy and resulting increased left ventricular mass.

Magnetic resonance angiography (MRA) is a group of techniques based on magnetic resonance imaging (MRI) to image blood vessels. Magnetic resonance angiography is used to generate images of arteries in order to evaluate them for stenosis, occlusions, aneurysms or other abnormalities. MRA is often used to evaluate the arteries of the neck and brain, the thoracic and abdominal aorta, the renal arteries, and the legs.
Coronary artery anomalies are variations of the coronary circulation, affecting <1% of the general population. Symptoms include chest pain, shortness of breath and syncope, although cardiac arrest may be the first clinical presentation. Several varieties are identified, with a different potential to cause sudden cardiac death.

Myocardial perfusion imaging or scanning is a nuclear medicine procedure that illustrates the function of the heart muscle (myocardium).
MRI contrast agents are contrast agents used to improve the visibility of internal body structures in magnetic resonance imaging (MRI). The most commonly used compounds for contrast enhancement are gadolinium-based contrast agents (GBCAs). Such MRI contrast agents shorten the relaxation times of nuclei within body tissues following oral or intravenous administration.
Perfusion is the passage of fluid through the lymphatic system or blood vessels to an organ or a tissue. The practice of perfusion scanning is the process by which this perfusion can be observed, recorded and quantified. The term perfusion scanning encompasses a wide range of medical imaging modalities.

Coronary artery aneurysm is an abnormal dilatation of part of the coronary artery. This rare disorder occurs in about 0.3–4.9% of patients who undergo coronary angiography.

Anomalous left coronary artery from the pulmonary artery is a rare congenital anomaly occurring in approximately 1 in 300,000 liveborn children. The diagnosis comprises between 0.24 and 0.46% of all cases of congenital heart disease. The anomalous left coronary artery (LCA) usually arises from the pulmonary artery instead of the aortic sinus. In fetal life, the high pressure in the pulmonic artery and the fetal shunts enable oxygen-rich blood to flow in the LCA. By the time of birth, the pressure will decrease in the pulmonic artery and the child will have a postnatal circulation. The myocardium, which is supplied by the LCA, will therefore be dependent on collateral blood flow from the other coronary arteries, mainly the RCA. Because the pressure in RCA exceeds the pressure in LCA a collateral circulation will increase. This situation ultimately can lead to blood flowing from the RCA into the LCA retrograde and into the pulmonary artery, thus forming a left-to-right shunt.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Cardiac magnetic resonance imaging perfusion, also known as stress CMR perfusion, is a clinical magnetic resonance imaging test performed on patients with known or suspected coronary artery disease to determine if there are perfusion defects in the myocardium of the left ventricle that are caused by narrowing of one or more of the coronary arteries.

Coronary CT angiography is the use of computed tomography (CT) angiography to assess the coronary arteries of the heart. The patient receives an intravenous injection of radiocontrast and then the heart is scanned using a high speed CT scanner, allowing physicians to assess the extent of occlusion in the coronary arteries, usually in order to diagnose coronary artery disease.
Cardiac imaging refers to minimally invasive imaging of the heart using ultrasound, magnetic resonance imaging (MRI), computed tomography (CT), or nuclear medicine (NM) imaging with PET or SPECT. These cardiac techniques are otherwise referred to as echocardiography, Cardiac MRI, Cardiac CT, Cardiac PET and Cardiac SPECT including myocardial perfusion imaging.
Raad Hashem Mohiaddin is professor of cardiovascular imaging at the National Heart and Lung Institute at Imperial College, London, and Royal Brompton Hospital. He is twice winner of the William S. Moore award of the International Society of Magnetic Resonance in Medicine the society's highest honor for medical investigators.

An MRI pulse sequence in magnetic resonance imaging (MRI) is a particular setting of pulse sequences and pulsed field gradients, resulting in a particular image appearance.