Medical ultrasound includes diagnostic techniques using ultrasound, as well as therapeutic applications of ultrasound. In diagnosis, it is used to create an image of internal body structures such as tendons, muscles, joints, blood vessels, and internal organs, to measure some characteristics or to generate an informative audible sound. The usage of ultrasound to produce visual images for medicine is called medical ultrasonography or simply sonography, or echography. The practice of examining pregnant women using ultrasound is called obstetric ultrasonography, and was an early development of clinical ultrasonography. The machine used is called an ultrasound machine, a sonograph or an echograph. The visual image formed using this technique is called an ultrasonogram, a sonogram or an echogram.

Cell adhesion is the process by which cells interact and attach to neighbouring cells through specialised molecules of the cell surface. This process can occur either through direct contact between cell surfaces such as cell junctions or indirect interaction, where cells attach to surrounding extracellular matrix, a gel-like structure containing molecules released by cells into spaces between them. Cells adhesion occurs from the interactions between cell-adhesion molecules (CAMs), transmembrane proteins located on the cell surface. Cell adhesion links cells in different ways and can be involved in signal transduction for cells to detect and respond to changes in the surroundings. Other cellular processes regulated by cell adhesion include cell migration and tissue development in multicellular organisms. Alterations in cell adhesion can disrupt important cellular processes and lead to a variety of diseases, including cancer and arthritis. Cell adhesion is also essential for infectious organisms, such as bacteria or viruses, to cause diseases.
Cell adhesion molecules (CAMs) are a subset of cell surface proteins that are involved in the binding of cells with other cells or with the extracellular matrix (ECM), in a process called cell adhesion. In essence, CAMs help cells stick to each other and to their surroundings. CAMs are crucial components in maintaining tissue structure and function. In fully developed animals, these molecules play an integral role in generating force and movement and consequently ensuring that organs are able to execute their functions normally. In addition to serving as "molecular glue", CAMs play important roles in the cellular mechanisms of growth, contact inhibition, and apoptosis. Aberrant expression of CAMs may result in a wide range of pathologies, ranging from frostbite to cancer.

Selectin P ligand, also known as SELPLG or CD162, is a human gene.

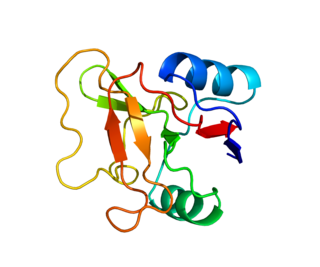
The selectins are a family of cell adhesion molecules. All selectins are single-chain transmembrane glycoproteins that share similar properties to C-type lectins due to a related amino terminus and calcium-dependent binding. Selectins bind to sugar moieties and so are considered to be a type of lectin, cell adhesion proteins that bind sugar polymers.
A contrast agent is a substance used to increase the contrast of structures or fluids within the body in medical imaging. Contrast agents absorb or alter external electromagnetism or ultrasound, which is different from radiopharmaceuticals, which emit radiation themselves. In x-ray imaging, contrast agents enhance the radiodensity in a target tissue or structure. In magnetic resonance imaging, contrast agents shorten the relaxation times of nuclei within body tissues in order to alter the contrast in the image.
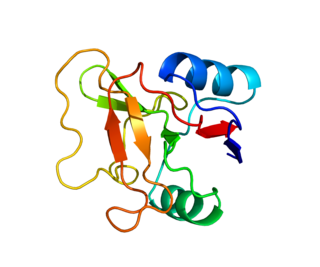
L-selectin, also known as CD62L, is a cell adhesion molecule found on the cell surface of leukocytes, and the blastocyst. It is coded for in the human by the SELL gene. L-selectin belongs to the selectin family of proteins, which recognize sialylated carbohydrate groups containing a Sialyl LewisX (sLeX) determinant. L-selectin plays an important role in both the innate and adaptive immune responses by facilitating leukocyte-endothelial cell adhesion events. These tethering interactions are essential for the trafficking of monocytes and neutrophils into inflamed tissue as well as the homing of lymphocytes to secondary lymphoid organs. L-selectin is also expressed by lymphoid primed hematopoietic stem cells and may participate in the migration of these stem cells to the primary lymphoid organs. In addition to its function in the immune response, L-selectin is expressed on embryonic cells and facilitates the attachment of the blastocyst to the endometrial endothelium during human embryo implantation.

E-selectin, also known as CD62 antigen-like family member E (CD62E), endothelial-leukocyte adhesion molecule 1 (ELAM-1), or leukocyte-endothelial cell adhesion molecule 2 (LECAM2), is a selectin cell adhesion molecule expressed only on endothelial cells activated by cytokines. Like other selectins, it plays an important part in inflammation. In humans, E-selectin is encoded by the SELE gene.
Targeted drug delivery, sometimes called smart drug delivery, is a method of delivering medication to a patient in a manner that increases the concentration of the medication in some parts of the body relative to others. This means of delivery is largely founded on nanomedicine, which plans to employ nanoparticle-mediated drug delivery in order to combat the downfalls of conventional drug delivery. These nanoparticles would be loaded with drugs and targeted to specific parts of the body where there is solely diseased tissue, thereby avoiding interaction with healthy tissue. The goal of a targeted drug delivery system is to prolong, localize, target and have a protected drug interaction with the diseased tissue. The conventional drug delivery system is the absorption of the drug across a biological membrane, whereas the targeted release system releases the drug in a dosage form. The advantages to the targeted release system is the reduction in the frequency of the dosages taken by the patient, having a more uniform effect of the drug, reduction of drug side-effects, and reduced fluctuation in circulating drug levels. The disadvantage of the system is high cost, which makes productivity more difficult, and the reduced ability to adjust the dosages.
Lymphocyte homing receptors are cell adhesion molecules expressed on lymphocyte cell membranes that recognize addressins on target tissues. Lymphocyte homing refers to adhesion of the circulating lymphocytes in blood to specialized endothelial cells within lymphoid organs. These diverse tissue-specific adhesion molecules on lymphocytes and on endothelial cells contribute to the development of specialized immune responses.

Leukocyte extravasation is the movement of leukocytes out of the circulatory system and towards the site of tissue damage or infection. This process forms part of the innate immune response, involving the recruitment of non-specific leukocytes. Monocytes also use this process in the absence of infection or tissue damage during their development into macrophages.

Echogenicity or echogeneity is the ability to bounce an echo, e.g. return the signal in medical ultrasound examinations. In other words, echogenicity is higher when the surface bouncing the sound echo reflects increased sound waves. Tissues that have higher echogenicity are called "hyperechogenic" and are usually represented with lighter colors on images in medical ultrasonography. In contrast, tissues with lower echogenicity are called "hypoechogenic" and are usually represented with darker colors. Areas that lack echogenicity are called "anechogenic" and are usually displayed as completely dark.
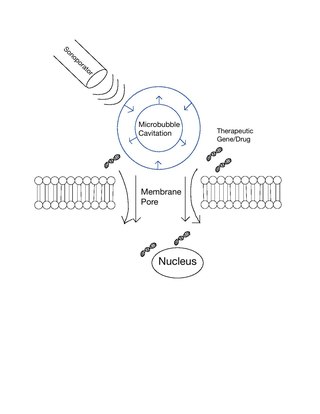
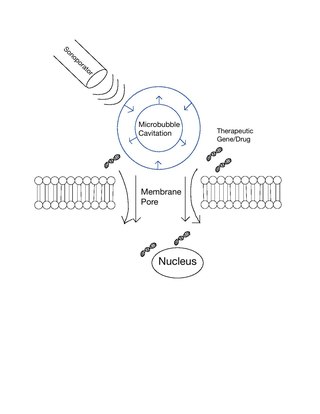
Sonoporation, or cellular sonication, is the use of sound in the ultrasonic range for increasing the permeability of the cell plasma membrane. This technique is usually used in molecular biology and non-viral gene therapy in order to allow uptake of large molecules such as DNA into the cell, in a cell disruption process called transfection or transformation. Sonoporation employs the acoustic cavitation of microbubbles to enhance delivery of these large molecules. The exact mechanism of sonoporation-mediated membrane translocation remains unclear, with a few different hypotheses currently being explored.
Microbubbles are bubbles smaller than one hundredth of a millimetre in diameter, but larger than one micrometre. They have widespread application in industry, medicine, life science, and food technology. The composition of the bubble shell and filling material determine important design features such as buoyancy, crush strength, thermal conductivity, and acoustic properties.
Preclinical imaging is the visualization of living animals for research purposes, such as drug development. Imaging modalities have long been crucial to the researcher in observing changes, either at the organ, tissue, cell, or molecular level, in animals responding to physiological or environmental changes. Imaging modalities that are non-invasive and in vivo have become especially important to study animal models longitudinally. Broadly speaking, these imaging systems can be categorized into primarily morphological/anatomical and primarily molecular imaging techniques. Techniques such as high-frequency micro-ultrasound, magnetic resonance imaging (MRI) and computed tomography (CT) are usually used for anatomical imaging, while optical imaging, positron emission tomography (PET), and single photon emission computed tomography (SPECT) are usually used for molecular visualizations.
Alexander L. (Sasha) Klibanov is associate professor in the Division of Cardiovascular Medicine and Department of Biomedical Engineering at the University of Virginia. He specializes in the study of ultrasound and medical imaging techniques.
A specific branch of contrast-enhanced ultrasound, acoustic angiography is a minimally invasive and non-ionizing medical imaging technique used to visualize vasculature. Acoustic angiography was first developed by the Dayton Laboratory at North Carolina State University and provides a safe, portable, and inexpensive alternative to the most common methods of angiography such as Magnetic Resonance Angiography and Computed Tomography Angiography. Although ultrasound does not traditionally exhibit the high resolution of MRI or CT, high-frequency ultrasound (HFU) achieves relatively high resolution by sacrificing some penetration depth. HFU typically uses waves between 20 and 100 MHz and achieves resolution of 16-80μm at depths of 3-12mm. Although HFU has exhibited adequate resolution to monitor things like tumor growth in the skin layers, on its own it lacks the depth and contrast necessary for imaging blood vessels. Acoustic angiography overcomes the weaknesses of HFU by combining contrast-enhanced ultrasound with the use of a dual-element ultrasound transducer to achieve high resolution visualization of blood vessels at relatively deep penetration levels.

Focused ultrasound for intracrainial drug delivery is a non-invasive technique that uses high-frequency sound waves to disrupt tight junctions in the blood–brain barrier (BBB), allowing for increased passage of therapeutics into the brain. The BBB normally blocks nearly 98% of drugs from accessing the central nervous system, so FUS has the potential to address a major challenge in intracranial drug delivery by providing targeted and reversible BBB disruption. Using FUS to enhance drug delivery to the brain could significantly improve patient outcomes for a variety of diseases including Alzheimer's disease, Parkinson's disease, and brain cancer.

A ligand-targeted liposome (LTL) is a nanocarrier with specific ligands attached to its surface to enhance localization for targeted drug delivery. The targeting ability of LTLs enhances cellular localization and uptake of these liposomes for therapeutic or diagnostic purposes. LTLs have the potential to enhance drug delivery by decreasing peripheral systemic toxicity, increasing in vivo drug stability, enhancing cellular uptake, and increasing efficiency for chemotherapeutics and other applications. Liposomes are beneficial in therapeutic manufacturing because of low batch-to-batch variability, easy synthesis, favorable scalability, and strong biocompatibility. Ligand-targeting technology enhances liposomes by adding targeting properties for directed drug delivery.
Theranostics, also known as theragnostics, is a technique in personalised medicine and nuclear medicine where a one radioactive drug is used to identify (diagnose) and a second radioactive drug is used to treat cancerous tumors.