Congenital iodine deficiency syndrome (CIDS) is a medical condition present at birth marked by impaired physical and mental development, due to insufficient thyroid hormone (hypothyroidism) often caused by insufficient dietary iodine during pregnancy. It is one cause of underactive thyroid function at birth, called congenital hypothyroidism, historically referred to as cretinism (obsolete). If untreated, it results in impairment of both physical and mental development. Symptoms may include goiter, poor length growth in infants, reduced adult stature, thickened skin, hair loss, enlarged tongue, a protruding abdomen; delayed bone maturation and puberty in children; and mental deterioration, neurological impairment, impeded ovulation, and infertility in adults.

A goitre, or goiter, is a swelling in the neck resulting from an enlarged thyroid gland. A goitre can be associated with a thyroid that is not functioning properly.

Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.
Liver tumors are abnormal growth of liver cells on or in the liver. Several distinct types of tumors can develop in the liver because the liver is made up of various cell types. Liver tumors can be classified as benign (non-cancerous) or malignant (cancerous) growths. They may be discovered on medical imaging, and the diagnosis is often confirmed with liver biopsy. Signs and symptoms of liver masses vary from being asymptomatic to patients presenting with an abdominal mass, hepatomegaly, abdominal pain, jaundice, or some other liver dysfunction. Treatment varies and is highly specific to the type of liver tumor.
Radiocontrast agents are substances used to enhance the visibility of internal structures in X-ray-based imaging techniques such as computed tomography, projectional radiography, and fluoroscopy. Radiocontrast agents are typically iodine, or more rarely barium sulfate. The contrast agents absorb external X-rays, resulting in decreased exposure on the X-ray detector. This is different from radiopharmaceuticals used in nuclear medicine which emit radiation.
Poppyseed oil is an edible oil obtained from poppy seeds.

Iodised salt is table salt mixed with a minute amount of various salts of the element iodine. The ingestion of iodine prevents iodine deficiency. Worldwide, iodine deficiency affects about two billion people and is the leading preventable cause of intellectual and developmental disabilities. Deficiency also causes thyroid gland problems, including endemic goitre. In many countries, iodine deficiency is a major public health problem that can be cheaply addressed by purposely adding small amounts of iodine to the sodium chloride salt.
Embolization refers to the passage and lodging of an embolus within the bloodstream. It may be of natural origin (pathological), in which sense it is also called embolism, for example a pulmonary embolism; or it may be artificially induced (therapeutic), as a hemostatic treatment for bleeding or as a treatment for some types of cancer by deliberately blocking blood vessels to starve the tumor cells.
Transcatheter arterial chemoembolization (TACE) is a minimally invasive procedure performed in interventional radiology to restrict a tumor's blood supply. Small embolic particles coated with chemotherapeutic drugs are injected selectively through a catheter into an artery directly supplying the tumor. These particles both block the blood supply and induce cytotoxicity, attacking the tumor in several ways.
Iodine deficiency is a lack of the trace element iodine, an essential nutrient in the diet. It may result in metabolic problems such as goiter, sometimes as an endemic goiter as well as congenital iodine deficiency syndrome due to untreated congenital hypothyroidism, which results in developmental delays and other health problems. Iodine deficiency is an important global health issue, especially for fertile and pregnant women. It is also a preventable cause of intellectual disability.
The Jod-Basedow effect is hyperthyroidism following administration of iodine or iodide, either as a dietary supplement, for iodinated contrast medical imaging, or as a medication.

Toxic multinodular goiter (TMNG), also known as multinodular toxic goiter (MNTG), is an active multinodular goiter associated with hyperthyroidism.
Hepatectomy is the surgical resection of the liver. While the term is often employed for the removal of the liver from a liver transplant donor, this article will focus on partial resections of hepatic tissue and hepatoportoenterostomy.

Hepatocellular adenoma is a rare, benign liver tumor. It most commonly occurs in people with elevated systemic levels of estrogen, classically in women taking estrogen-containing oral contraceptive medication.

Liver cancer, also known as hepatic cancer, primary hepatic cancer, or primary hepatic malignancy, is cancer that starts in the liver. Liver cancer can be primary in which the cancer starts in the liver, or it can be liver metastasis, or secondary, in which the cancer spreads from elsewhere in the body to the liver. Liver metastasis is the more common of the two liver cancers. Instances of liver cancer are increasing globally.

Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radionuclide therapy used in interventional radiology to treat cancer. It is generally for selected patients with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver. The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor. Because this treatment combines radiotherapy with embolization, it is also called radioembolization. The chemotherapeutic analogue is called chemoembolization, of which transcatheter arterial chemoembolization (TACE) is the usual form.
Yttrium-90 is a radioactive isotope of yttrium. Yttrium-90 has found a wide range of uses in radiation therapy to treat some forms of cancer. Along with other isotopes of yttrium, it is sometimes called radioyttrium.
Interventional oncology is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments to allow targeted and precise treatment of solid tumours located in various organs of the human body, including but not limited to the liver, kidneys, lungs, and bones. Interventional oncology treatments are routinely carried out by interventional radiologists in appropriate settings and facilities.
Iodine is a chemical element with many uses in medicine, depending on the form. Elemental iodine and iodophors are topical antiseptics. Iodine, in non-elemental form, functions as an essential nutrient in human biology. Organic compounds containing iodine are also useful iodinated contrast agents in X-ray imaging.
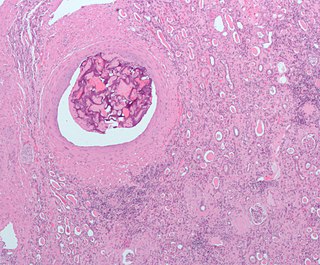
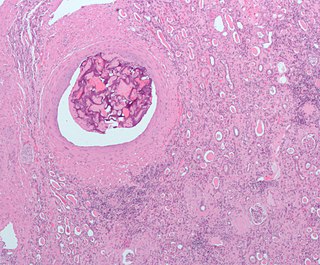
Transarterial bland embolization is a catheter-based tumor treatment of the liver. In this procedure, embolizing agents can be delivered through the tumor's feeding artery in order to completely occlude the tumor's blood supply. The anti-tumor effects are solely based on tumor ischemia and infarction of tumor tissue, as no chemotherapeutic agents are administered. The rationale for the use of bland embolization for hepatocellular carcinoma (HCC) and/or other hyper-vascular tumors is based on the fact that a normal liver receives a dual blood supply from the hepatic artery (25%) and the portal vein (75%). As the tumor grows, it becomes increasingly dependent on the hepatic artery for blood supply. Once a tumor nodule reaches a diameter of 2 cm or more, most of the blood supply is derived from the hepatic artery. Therefore, bland embolization and transarterial chemoembolization (TACE) consist of the selective angiographic occlusion of the tumor arterial blood supply with a variety of embolizing agents, with or without the precedence of local chemotherapy infusion. The occlusion by embolic particles results in tumor hypoxia and necrosis, without affecting the normal hepatic parenchyma.